Labor of love

AirMed&Rescue spoke with Redstar Aviation Medical Director, Dr Joseph Choi, about maintaining standards and what the future may hold
What is your background in the air medical industry, and what made you want to work in this sector?
My first experience was 12 years ago when I was tasked as a medical escort on a commercial flight for a stretcher patient. Honestly, I was unaware that such a service and industry existed until I started working at a major medical and travel assistance company – and I was sort of thrust into it, as opposed to it being a childhood dream. But I’m very thankful and fortunate that it turned out the way it did, as I’d always fostered a special interest in aviation. After a couple of years of commercial escorting, I had the privilege to board a dedicated air ambulance aircraft – a Redstar Aviation Jetstream 32EP. Although it had a spacious cabin, its performance and range allowed limited regional operations, due to it being a turboprop, but it certainly served as a venue for some of my most memorable air ambulance experiences. The addition of the Learjet 45 to our fleet in 2015 opened doors to a much wider geography and clinical scope, further expanded by the introduction of the Challenger 605 aircraft in 2021.
What has been the biggest Covid-19 challenge from an air medical transfer point of view? Has it been managing infectious patients, or the logistics of organizing the flights themselves into countries with strict border controls?
By far, it was trying to help as many Covid patients as possible, while protecting our medical and flight crews. Especially during the early days of the pandemic, when there was uncertainty, fear and more lethal variants of the virus.
But we enjoyed the benefit of being well prepared prior to the pandemic, having already provided such services for various governmental and non-governmental organizations. Our operational and medical infrastructure – in terms of staff and equipment – was ready to face Covid-19 when it all began. Our aircraft has state-of-the-art additional medical equipment, such as next-generation isolation pods and chambers, to provide maximum protection and safety for both the contaminated patients and our team.
Hygiene is also taken very seriously. Each aircraft is thoroughly cleaned and detailed from the inside out, ensuring it is sanitized and ready to go for each trip throughout the day. All these actions are planned in detail and their management is based on our risk assessments conducted regularly during the pandemic, as the safety of patients and medical teams are our priority.

What trends are you seeing in the industry in terms of recovery to pre-pandemic levels of business for international fixed-wing air ambulances?
One of the major obstacles, with direct implications on patient care during the pandemic, was the inability to enter a country to perform a bedside patient pick-up/drop-off. At the peak of restrictions, air ambulance medical crew were not permitted to leave the tarmac and, in some geographies, the confines of the aircraft cabin. With this being eased in much of the world, we are practically back to pre-pandemic levels of bed-to-bed transfers, which is without a doubt in the best interests of the patient.
In addition to the fixed-wing air ambulances, Redstar Aviation offers offshore support to the oil and gas industry. What are the daily issues you face for this part of the company specifically?
Offshore platforms are high-risk environments and our medical crew needs to be alert and responsive 24/7 for anything that could go wrong. Thankfully, a major incident is far from a daily occurrence, but our crew has to be physically and mentally ready for any accident or medical issue on the platforms. This also means night operations with a helicopter, which can be a dangerous combination.
What is Redstar’s fleet composition, and do you have a different medical crew for each type of aircraft?
Our fleet is comprised of six dedicated fixed-wing air ambulance aircraft: four Learjet 45 and two Challenger 605. Our standard crew composition for both, flying a single patient, is a doctor and nurse with emergency/critical care background. Depending on the patient, this standard crew might be augmented with a third medical crew member. On rare and complex occasions (e.g. ECMO patients), a fourth individual could even be tasked. Another determinant of crew composition is the number of patients onboard. Every fixed-wing aircraft in our fleet is configured with double ICU stretchers. In situations where extra patients require transportation, we may accommodate more than two, if at least one of them is able to be seated. Crew composition for each scenario would need to cover for simultaneous care needs of each patient.

In terms of medical equipment, what do you consider the most essential, and what do you carry that is non-essential, but extremely useful?
With the addition of the CL605 to our fleet, we have noticed a meaningful increase in the average flight time with patient. Point-of-care devices able to display critical laboratory values – such as blood gases, electrolytes and metabolites – are certainly essential pieces of equipment, especially when time spent outside of a hospital setting is prolonged. Scissors are perhaps one of the least technologically advanced pieces of equipment onboard, but they have proven their value and have a special place among our medical crews!
Do you carry out wing-to-wing transfers, and if so, how do you ensure the highest standards of patient care at all times?
We try to perform every mission from start to finish by our own means of aircraft and crew as much as possible. This ensures a minimum change of hands and equipment, delivering as much uninterrupted patient care as we can. However, this is not always possible, especially in long-distance flights crossing multiple time zones. When we do carry out wing-to-wing transfers, we want to select a provider that shares our common vision in terms of quality and safety (e.g. EURAMI accreditation). All of the relevant medical information, observations and interventions performed during the journey needs to be handed over in detail. A briefing with the wing-to-wing partner in the planning stages, alongside continued communication of the patient’s medical situation throughout the mission, can be very beneficial in ensuring that everyone involved is on the same page.
What is the most challenging case you’ve flown, and why was it more difficult than most?
We have certainly encountered our fair share of challenging missions. I cannot single out one specific instance, but rescuing patients from countries with active conflicts – such as Afghanistan, Libya, Yemen and Somalia – is often clinically very challenging, due to the available infrastructure and resources, as well as concerns around the safety and welfare of our crew and assets.
January 2023
Issue
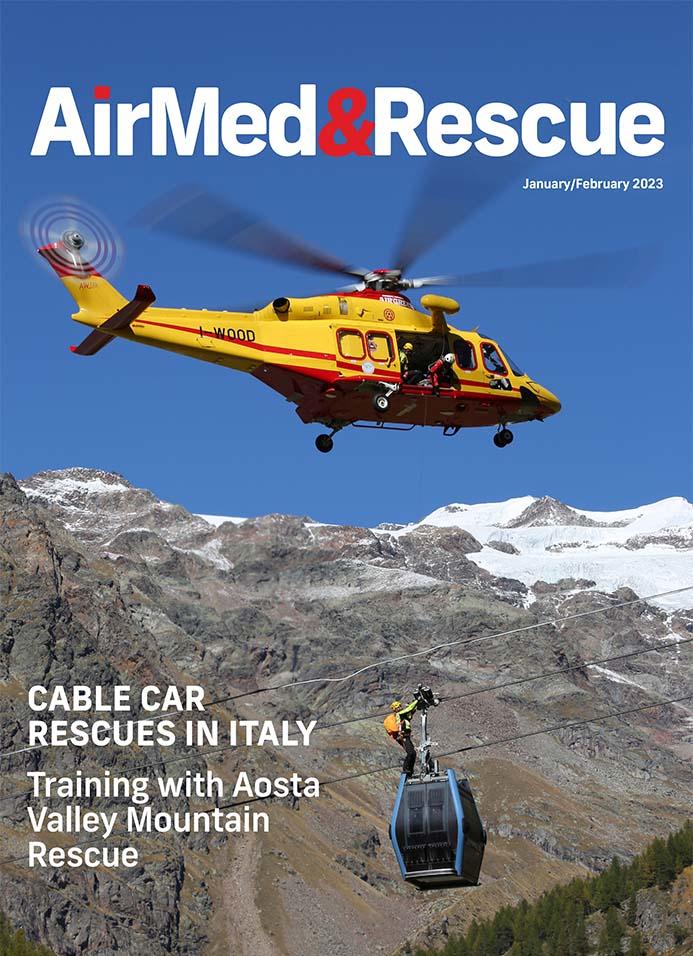
In the January/February 2023 issue
Technology to aid, enhance and support you in the cockpit; how do HEMS operators around the world approach SAR with different rules and technology; what do people know about AA: who can access it, when can they use it, how much does it cost, and how is it funded; plus a whole lot more to keep you informed and good to go!
Editorial Team
The AirMed&Rescue Editorial Team works on the website to ensure timely and relevant news is online every day. With extensive experience and in-depth knowledge of the air medical and air rescue industries, the team is ready to respond to breaking industry news and investigate topics of interest to our readers.



