Changing the perceptions of air ambulance operations

Funding and general awareness of the air ambulance sector varies widely around the world. How do services survive and what can the aeromedical industry do to increase popular understanding? Jonathan Falconer spoke to UK and overseas operators to learn more about the differences in public perception and funding models
Correcting misconceptions
There is still some mistaken thinking out there that air ambulances are paid for by the state and are a ‘scoop and go’ service, simply flying patients to the most appropriate hospital as quickly as possible, then ‘drop and run’ before returning to base. These misconceptions could not be further from the truth.
“As part of a recent survey, Midlands Air Ambulance Charity (MAAC) found that little more than 30 per cent of those questioned in the UK were still not aware of the enhanced clinical skillset, advanced medicines and hospital-level equipment that MAAC carries directly and rapidly to incident scenes,” revealed Emma Gray, the UK charity’s Chief Operating Officer.
However, MAAC’s service uses three helicopters (two EC135s and one H145) and is much more than that: “The enhanced clinical team bring parts of the hospital Emergency Department directly to the patient, in some instances giving them the definitive care required, before then transferring them to hospital,” said Gray. “It may mean spending longer at the incident scene, but the care provides patients with the best chance of survival and better recovery outcomes.”
Redstar Aviation’s longstanding aeromedical experience of more than 33 years means its service is prominent with Turkish domestic users, as well as corporate and governmental clients. “With our fleet of six Challenger 605 and Learjet 45XR dedicated air ambulances, we offer services to a worldwide clientele consisting of major insurance, medical assistance companies and governmental organizations. Since we are well-known to many health institutions as an air ambulance provider, we are easily accessible to the users,” said Redstar’s spokesperson.
In East Africa, Nairobi-based AMREF Flying Doctors (AFD) air ambulance service is seen by the Kenyan public as expensive and out of reach of the ordinary individual, as Dr Joseph Lelo, Medical Director of AFD, explained: “It is perceived as being mainly for tourists or travellers in the region who may get sick or injured while in remote parts of Africa, and require rescue flights to hospitals for initial care and then to be flown back home on repatriation missions.” AFD operates a fleet of six aircraft, providing medical evacuation services throughout the Eastern Africa region, comprising three jets (Citation Bravo C550, XLS C560 and Sovereign C680), one turboprop Pilatus PC12 and a single Eurocopter AS350.
Australians have an altogether different take on air medical prehospital and interhospital services, which are embedded in the expectations of basic healthcare rights in Australia. “Since the inception of the Royal Flying Doctor Service in 1928, rural and remote Australians have embraced the philosophy that air medicine is a ‘mantle of safety’ that should support access to care for a very geographically dispersed population, irrespective of location,” commented Dr Mardi Steere, Executive General Manager, Medical & Retrieval Services with Australia’s Royal Flying Doctor Service Central Operations (RFDS).
Australians have an altogether different take on air medical prehospital and interhospital services
A communication strategy
So, what can the air medical sector do to get the message out there to help people understand more about the nature of air ambulance operations?
Gray believes that regular and simplified communication to supporters and donors ‘demonstrates how the important and life-saving work of air ambulances is vital to retaining and gaining new support, as well as appealing to the clinicians and pilots of tomorrow to strive to work for a HEMS platform.’ “As a sector, every September in the UK, Air Ambulance Week is organised by Air Ambulances UK to demonstrate nationally what the air medical sector does to help the public get a better understanding of what we can bring to scene,” said Gray.

AFD is boosting the Kenyan public’s perception of its operations through the introduction of a low-cost membership scheme. “This allows access to emergency medevac flights at no extra cost,” said Dr Lelo. “This has been very well received for the peace of mind it gives and the low-cost, ‘no-frills’ access to a professional air ambulance service,” he added. AFD is also proactively involved in disaster response and other community activities, which are helping raise public awareness of the organization’s air medical services. “Lobbying and media events, public fairs and airshows also present opportunities to showcase and educate the public about air ambulance services,” said Dr Lelo.
Covid-19 did much to educate the Turkish population about the nature of air ambulance work. “Increased demand for air medical services during and after the pandemic expanded the use of air ambulances in Turkey, as well as globally,” revealed Redstar. “Private medical transfers were demanded more frequently during this period, with low mobility due to travel restrictions. Patients with Covid symptoms and in need of emergency treatment began to prefer air ambulance to reach medical institutions.”
The Redstar spokesperson described how an unanticipated consequence of the pandemic has been the huge increase in internet use to find out information, buy goods and services, and for communication. This has led to a growing awareness among the public of the nature of air medical services and what they can offer, manifesting itself in a significant uptick in consumers accessing air ambulance companies. “The patients or their relatives can easily reach out to air ambulance providers in Turkey – and they choose this service even if it is high-priced, especially when advanced treatment is needed. As a result, the popularity of this service increases every day."
Dr Steere takes a different view: “There is a risk that air medicine can be perceived purely as an adrenaline sport for thrill-seeking clinicians,” she maintained. “And stories of, for example, myriad rotary providers competing for market share in dense American cities don’t help that perception,” she said.
Different countries, different funding
There are 22 air ambulance organisations across the UK; all but one of which are charitable, that neither receive nor seek government, National Health Service (NHS) or National Lottery funding. Scotland is the only country in the Union to have NHS-funded air ambulance provision.
“Midlands Air Ambulance Charity attends approximately 4,500 incidents via our three air ambulances and three critical care cars each year, relying on donations from the public and local businesses to fund our daily missions,” said Gray. “As such, our fundraising is from sources such as committed giving and ad hoc donations from the community and corporate sector.”
MAAC needs to raise £11 million each year to keep its life-saving, prehospital emergency service operational. The funding for daily missions is raised through community and corporate donations, legacy giving, committed giving, charity shops, grants and investments. “In the past, the charity has also received one-off funding contributions towards two capital projects – the purchase of one of our aircraft and for its upcoming new airbase, headquarters and training facility – which are dedicated to future-proofing its life-saving service,” commented Gray.
Turkey – commercial, but also free of charge to citizens
Air ambulance services in Turkey are offered to customers by private companies such as Redstar Aviation, which is one of a number of commercial operators providing air medical services direct to the consumer. In Turkey, air ambulances are a business and charitable funding is not used.
The company explained: “An air ambulance service in Turkey is offered by the state to its citizens free at the point of use, unlike other European countries, especially England. The Turkish government has no air ambulance aircraft of its own, so provides this service to its citizens by purchasing it from third-party private providers like Redstar. In this context, the state is able to call on a large number of fixed- and rotary-wing air ambulances to provide this service.”

“Although they do not have the size of our fleet, other air ambulance companies with one or two aircraft can provide these services locally and regionally too,” said Redstar. Using Turkey’s broad network of air medical brokers, service requests are shared with multiple air ambulance providers simultaneously. “For this reason, when compared to other countries, the charitable funding system does not exist in Turkey. The companies that provide this service offer it as a totally commercially focused operation,” the spokesperson said.
“Usually, service requests come from the health institutions where the patients are being treated or through the doctors,” continued Redstar's representative. “Besides that, users who have knowledge about the service can reach companies through various marketing and sales channels such as websites and social media platforms,” he continued.
AFD may occasionally get donations from a well-wisher to support its charity medevac activities, but this contributes less than one per cent of revenue
Due to the large area of the country (302,535m2), fixed-wing aircraft are usually preferred for long-range transfers such as east-west (995 miles) or north-south (404 miles), especially to big cities like Istanbul, Ankara and Izmir, where medical facilities are better equipped. Helicopters are preferred for transfers from rural or remote areas to city centers. From time to time, medium-range flights operated by multiple helicopters are also undertaken.
Kenya – for-profit and social enterprise
Dr Lelo: “AFD is a self-funded social enterprise. Our medevac activities generate a surplus, which provides a much-needed source of unrestricted funding for our parent organization, AMREF Health Africa. Other operators are either for-profit privately-owned companies or donor-funded charities,” he reported.
Dr Steere lived in Kenya from 2011 to 2019, volunteering at Kijabe Hospital in Paediatric Emergency and becoming Director of Clinical Services, before returning to her native Australia for an executive role with RFDS. She gives an additional insight into the commercial basis in Kenya: “The prehospital and interhospital services, including both road and air ambulance, are performed by private companies, which require membership or a pay-as-you-go model, which are not financially accessible by the majority of Kenyans,” she revealed.
AFD may occasionally get donations from a well-wisher to support its charity medevac activities, but this contributes less than one per cent of revenue. “Our main source is paid-for flights by insurers or individuals and our membership scheme,” commented Dr Lelo.
Australia – a hybrid system
Funding of air ambulance services in Australia is as varied as the topography of this vast continent, as Dr Steere pointed out: “RFDS has a hybrid government/community funding model, relying on a committed donor and corporate partner base, while other air medical providers around the country vary from not-for-profit organizations with similar funding models, to for-profit companies supplying aircraft and crews for state-based ambulance authorities and retrieval teams.”
Not-for-profit operators include CareFlight in the Northern Territory (NT) and LifeFlight in Queensland (QLD), with for-profits like Toll and Pel-Air providing services for Victoria and New South Wales (NSW). All have state government contracts to provide retrieval services (NT and QLD) or aircraft/crews for Toll and Pel-Air, in partnership with clinicians from Ambulance Victoria or NSW Air Ambulance.
“RFDS relies on its hybrid funding mainly for CAPEX (including fleet replacement, aviation infrastucture and regional patient transfer facilities), with OPEX primarily funded through multiple contracts with state, federal and other health partners, for whom we are an integrated link in a chain of a broader service and strategy,” explained Dr Steere.
Last word
Dr Steere’s view is that conversations about health equity really should underpin the value proposition of air medicine. It’s an argument that could as easily apply to other countries, where the provision of air ambulance services is either dependent on charitable funding or devoid of direct state support.
“In Australia, if we instead focus on outcomes, there is measurable value at a public health level for rural and remote populations when time to definitive care can drop by hours, rather than minutes, due to the provision of prehospital and interhospital air medical services,” she declared.
January 2023
Issue
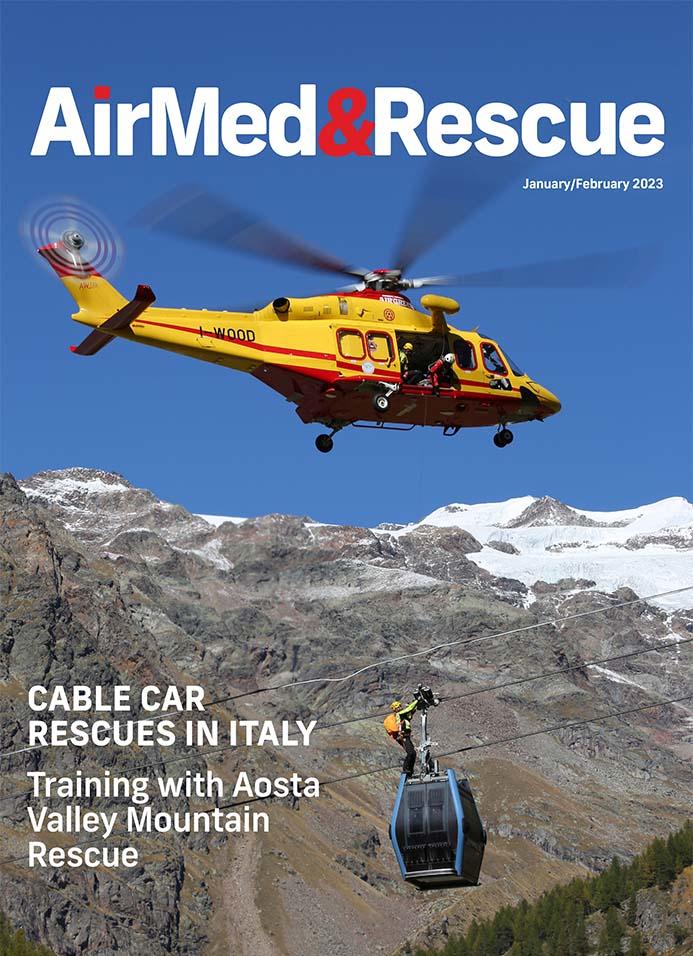
In the January/February 2023 issue
Technology to aid, enhance and support you in the cockpit; how do HEMS operators around the world approach SAR with different rules and technology; what do people know about AA: who can access it, when can they use it, how much does it cost, and how is it funded; plus a whole lot more to keep you informed and good to go!
Jonathan Falconer
With many years as a publishing and editing professional under his belt, former Senior Editor with AirMed&Rescue, Jonathan continues as a freelance contributor. He was previously the Senior Commissioning Editor, Aviation & Military Titles, for Haynes Publishing. A keen aviation and military enthusiast, he brings a wealth of knowledge to the table.




