Taking stroke detection into the skies

Ground-breaking new airborne lightweight CT scanners are under competitive development by the Australian Stroke Alliance. Jonathan Falconer reports on how the idea of taking diagnosis and treatment to the patient via aeromedical retrieval promises a leap forward in how stroke is diagnosed and treated in a pre-hospital setting
Stroke is a medical condition affecting one in four adults worldwide over the age of 25. A staggering 13.7 million people globally will suffer their first stroke this year and 5.5 million will die as a result.
The incidence of stroke increases substantially with age.
It is a condition where the blood supply to the brain is disrupted by a clot in an artery, resulting in oxygen starvation, brain damage and loss of function. It can also be caused by hemorrhage when a burst vessel causes blood to leak into the brain. One of the main disease processes leading to stroke is atherosclerosis – a thickening or hardening of the arteries caused by a build-up of plaque on the inner lining of the vessels.
Stroke can cause permanent damage, including partial paralysis and impairment in speech, comprehension, and memory. The severity of the stroke, which can range from minimal to catastrophic, is determined by the extent and location of the damage in the brain.
First responders know that intervention in the ‘Stroke Golden Hour’ can make a lifetime’s difference as brain cells begin to die.
In the last 20 years, improved medications and surgical interventions have transformed stroke care – clot-busting drugs and surgical clot removal can stop the damage in its tracks, with quite extraordinary results when delivered within the first few hours of the stroke.
Taking the CT scanner to the stroke patient
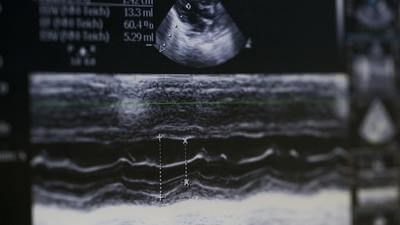
We know how to treat a stroke, but a paradigm shift is now taking place in how it is diagnosed and treated within the first ‘Golden Hour’ – by taking the computerized tomography (CT) scanner to the patient in an air ambulance. By determining whether the cause is a clot or a bleed and initiating the correct treatment before arrival at a hospital, longer-term damage can be mitigated and the patient’s outcome dramatically improved.
At the cutting edge of this bold initiative – which can be compared to the revolution that took place in cardiac intervention when defibrillators and electrocardiograms (ECG) were placed in ambulances – is a team of biomedical engineers and doctors working with the Australian Stroke Alliance.
The Alliance’s research program is multi-faceted, encouraging three unique approaches to lightweight, portable, and affordable brain scanners
The Alliance’s research program is multi-faceted, encouraging three unique approaches to lightweight, portable, and affordable brain scanners.
“The idea to take diagnosis and treatment to the patient via HEMS and fixed-wing is based on the vast size and distribution of the population in Australia,” explained biomedical engineer Professor Kate Fox, Associate Dean in the School of Engineering at the Royal Melbourne Institute of Technology (RMIT), and a member of the Australian Stroke Alliance team.
Stroke is one of Australia’s biggest killers and a leading cause of disability. There is a stroke every nine minutes in Australia, which claims the lives of 12,000 people annually.

“At present, we have a disparity in the level of stroke detection and treatment for those patients that are not based in the main cities of Australia. In order to get a good patient outcome, a stroke needs to be diagnosed and treated within the first hour of symptoms (the ‘Golden Hour’) and thus access to remote populations by air or road ambulance do not provide the support needed. A road-based mobile stroke unit has been embedded in Melbourne with great success and now it is time to widen the net by taking stroke detection equipment to the sky,” explained Professor Fox.
Biomedical engineer Kern Cowell is a Research Fellow at RMIT and a Stroke Alliance team member. “As a medical engineer I thrive working on interesting and challenging problems with real-world application. Rural and regional locations throughout both Australia and the world do not have fast access to essential imaging to aid diagnosis and management. This therefore led to the development of road ambulance mobile stroke units and subsequently the work on developing a CT scanner for use in an aircraft,” he commented.
Weighty matters
CT scanners are substantial pieces of medical equipment and there is clearly a weight issue when considering how to carry one onboard a fixed-wing or helicopter air ambulance.
“A traditional scanner like you would find in hospitals is located in the basement for good reason,” said Professor Fox. “It is currently designed to be glued to the floor and the patient comes to it, not the other way round, so we are looking at ways to decrease the weight and redesign the scanner for transportation to the patient,” she revealed.
Dr Mardi Steere is the national clinical lead for this project for the Royal Flying Doctor Service (RFDS) of Australia: “Weight, space and flexibility are critical to any new service delivery on an aircraft,” she disclosed. “Every kilogram of extra weight equates to a 3km reduction in range on our fixed-wing Pilatus PC-12 fleet due to fuel usage. So, communicating what decreasing the weight and size of this machine needs to be, in terms of access for our most remote patients, is important.”
Dr Steere has helped to shape technology developers’ acceptance of the portability of the scanner in that it cannot be a hard-mounted device in every aircraft.
She asserted, “we can’t have these 50kg devices sitting onboard taking up space and fuel when we go out to retrieve a patient with sepsis; we need to be able to have it on base, ready to load for a specific patient, on any of our aircraft, and to move it from one plane to the next so that, for example, scheduled aircraft maintenance can occur.”

Three ways to solve a problem
Currently, there are three projects to design a lightweight mobile CT scanner running independently of one another. The first is the Alliance project, where Professor Fox has been working on stripping down an existing CT scanner in an attempt to produce a device light enough to fly.
Her modification would work in a similar way to the model found in Melbourne’s mobile stroke unit (road ambulance); the second is EM Vision’s perfusion-based electro-magnetic helmet scanner; and the third is Micro-X, with its CT nanotechnology-based ring scanner. “Each one has different approaches,” commented Dr Steere, “and all have great potential with some encouraging hospital-based results already being released. The next step will be proof-of-concept trials at a limited number of specific bases alongside those companies.”
Installation in aircraft
An aeromedical team at RMIT led by Professor Cees Bil is investigating the effect of vibration on any of the newly designed scanners as determined by the flight conditions and transportation type – fixed-wing and helicopter. “At a local level we need to make sure that as we decrease the weight and components, we still have a functional scanner under the challenging conditions of flight,” said Professor Fox.
Kern Cowell has a personal interest in developing a lightweight CT scanner suitable for HEMS use. “What motivates me is to work on problems that some would consider improbable or even impossible to solve, and that the solution will greatly benefit patients and improves people’s lives,” he revealed. “I have seen the devastating effects a stroke can have on a close family member, so when I heard about this project to provide faster stroke diagnosis, I had to take the opportunity to help other families such as mine.”
Kern is working on solutions to carry the scanner in a HEMS aircraft: “There are many technical hurdles that we are working to overcome, and like any complex problem we will undoubtedly discover new questions and challenges as the project progresses,” he said.
“The main hurdle we are working on is to reduce the weight of the scanner. We are doing this by removing components that are not essential to its function, redesigning components and replacing materials with lighter, stronger alternatives. However, changing the components and the materials changes its structural integrity. Therefore, we must also validate that the new scanner design can withstand the load conditions required, which will be done by a combination of computerized structural analysis (FEA) and mechanical testing.”
Once the scanner is as light as the team can make it, the next hurdle will be how to integrate the device into the aircraft itself. Kern continued: “The CT scanner will be fixed to the aircraft via the seat tracks, a vibration damping attachment plate will need to be designed to attach these together,” he commented.
“The current plan is to integrate a layer of damping material within the attachment plate to reduce vibration from the aircraft to the scanner while in flight, during take-off and during landing. The scanner itself runs from batteries held inside the unit and will charge from the auxiliary power of the aircraft. Patients will only be scanned when the aircraft is stationary on the ground.”
With a device that emits controlled radiation during its operation, there have been several compliance and safety requirements that needed addressing before the scanner can be taken into the air. “Small things like the helicopter needs to have its pilot in the vicinity of the controls while the [scanner] power is on are things that we had not considered at first,” commented Professor Fox.
“Safety of the pilot from radiation etc is paramount. And then, of course, we are now taking the scanner into central Australia where the temperature is high and the roads are dirt, which add new levels of complexity!” she said.

In the field
While the airborne stroke scanner heralds a bright new dawn in pre-hospital stroke diagnostics, it also comes with a
While the airborne stroke scanner heralds a bright new dawn in pre-hospital stroke diagnostics, it also comes with a remote data connectivity challenge
remote data connectivity challenge, as Dr Mardi Steere disclosed: “This is not like a city stroke ambulance. Our remote stroke patients could be on a cattle station, in a remote community, or on the side of a dirt road when we get to them, and that’s where we not only want to scan them, but send their images immediately through to a neurology team,” she explained. “So, at the same time as developing the scanner, we need to in parallel develop seamless data connectivity on our planes, which necessitates hardware and batteries (more kilograms!) and data costs.
Figuring how to do this cost effectively, both as a capital expenditure and as an operational one, is ongoing work for us in the background. And communicating to the equipment developers and stroke neurologists upfront that image size and compression really matter has been important from the first day. All of these things need to be developed from ground zero with those different interfaces in mind,” she emphasized.
Regulatory common sense
With such a sea-change on the horizon in resetting the inequalities in stroke care and patient management, Dr Mardi Steere is adamant that an intelligent regulatory framework must be in place for effective use of the stroke scanner. “Road stroke ambulances have the luxury of being able to send whichever clinicians and technicians seem to make the most sense. We have been communicating from the inception of the project that a retrieval team is two skilled clinicians and a pilot, maximum – whether that be a retrieval doc and flight nurse, two flight paramedics, or other combinations of retrieval clinicians,” asserted Dr Steere.
“Whatever device is proposed, we want to ensure that we have the regulatory approvals that do not limit its operation to a specific additional technician, or require a neurologist to be on board,” maintained Dr Steere. “Remote bases such as Kalgoorlie or Mount Isa will not have that luxury, so we need to be able to make this work with teams that are currently assigned to fixed-wing bases around the country, or it will not be adopted or accessible widely,” she warned.
Broad potential
Dr Mardi Steere observed that any lightweight equipment that has agility in its use has great potential, not just for fixed- and rotary-wing air ambulances, but also for road ambulance applications and remote clinics that have limited clinical staff on site.
“Over short distances, there is benefit in every minute saving brain cells, but over longer distances being able to either commence thrombolysis en route to hospital, or change the primary disposition of the patient to a thrombectomy-equipped tertiary center will have a huge impact on long-term morbidity and disability-adjusted life years (DALY),” said Dr Steere.
“When you consider large distances and limited access to care, places like Australia, Canada, sub-Saharan Africa, and other geographically dispersed populations could benefit massively by diagnosis and therapy being brought to them hours before they could get to help. And expanding the scope of this imaging beyond stroke to head trauma and other applications is also worth considering,” she envisioned.
Professor Fox: “As we look at the CT scanner and are finding new ways to decrease its weight, we are also opening up new ways to use the equipment. It provides an opportunity to take a lite scanner into more road applications, where specialist vehicles are no longer required to house the scanner, as well as moving the CT scanner out of hospital basements and into more parts of the hospital.”

A vision for the future
There is a bright future ahead for the lightweight CT scanner, thanks to the vision of the Australian Stroke Alliance team
This is not just about machines – this is about developing a ‘Stroke Ecosystem’
led by Professors Geoffrey Donnan and Stephen Davis, who attracted talent like Dr Steere to the research program. Dr Steere’s extensive clinical experience as a pediatric emergency physician in the US, Australia, and Kenya, and in aeromedical retrievals, has given her a unique vantage point from which to comment on how the stroke scanner fits into the bigger picture of managing stroke worldwide: “One of the most exciting things about this project is the system approach it has taken from the beginning.
This is not just about machines – this is about developing a ‘Stroke Ecosystem’. From education of remote practitioners in early recognition of stroke symptoms, to tertiary neurologists equipping remote centers with telehealth and harmonized scoring/reporting systems, to strengthening communication and referral pathways, to rapid response with diagnosis and treatment,” applauded Dr Steere.
“RFDS is very proud to be part of a health system that is working on the patient journey from the time they are feeling slightly off color to repatriating and rehabbing them at the end of their hospital journey – which is the start of a much longer recovery journey. This project is exciting when you look at the equipment – but the innovation in comprehensive care is in many ways more important, and hopefully a template for better outcomes in many illness and injury patterns we see in our rural, regional, and remote populations.”
October 2022
Issue
Aerial firefighting and SAR after 9/11; innovative use of stroke scanners by the RFDS; European nations’ response to this summer’s intense wildfire season; and the ongoing evolution of night vision systems, all in the latest issue. Plus, the USHST and EASA share regulatory updates on safety measures for operators, and the European Rescue Swimmers’ Association tells us what’s coming up at their next event
Jonathan Falconer
With many years as a publishing and editing professional under his belt, former Senior Editor with AirMed&Rescue, Jonathan continues as a freelance contributor. He was previously the Senior Commissioning Editor, Aviation & Military Titles, for Haynes Publishing. A keen aviation and military enthusiast, he brings a wealth of knowledge to the table.