Air ambulance medical equipment – what’s new?
Air medical professionals around the world shared their in-depth insights into latest developments in the medical equipment sector, including what equipment they need now and in the future
The investment in outfitting an air ambulance – whether fixed wing or rotary – is significant, and the decision to purchase a particular piece of medical equipment is not one to be taken lightly. Cost, efficacy, weight, and the difference it will make to patient outcomes are all important parts of the decision-making process.
Dr Bruno Sicard, former Chief Medical Officer for Allianz North America and now an auditor for the European Aero-Medical Institute (EURAMI), spoke to AirMed&Rescue about the current limitations in patient care facing aeromedical professionals, and what medical equipment could make a difference to outcomes in the future. “Realistically, nowadays, there are almost no limits to patient care onboard air ambulances and even commercial aircraft, thanks to advances in medical equipment such as Extra Corporeal Membrane Oxygenation (ECMO) and developments like Lufthansa’s Patient Transport Compartment, where even critical patients can be transported over long distances as long as they are stable,” he said. “What is lacking, though, is accurate and fast diagnostic equipment.”
While Covid-19 brought international travel to an abrupt end, borders are gradually opening again, meaning that people will travel – maybe not too far afield, and in lesser numbers until confidence is restored, but there is little doubt in the travel industry that long-haul travel will eventually return to previous levels. And when people travel, accidents and illnesses will happen. For fixed-wing air ambulance operators, it is this segment of travellers that forms the backbone of their business – and, as Sicard pointed out, transporting patients over longer distances means that their condition has a greater opportunity to change and, in such situations, the flight doctor or nurse needs to be able to accurately diagnose the new condition and then treat the patient accordingly. The longer the transport, the more chance the patient’s condition could change and the more equipment the air ambulance or medical escort needs to carry.

Dr Jörn Adler, Medical Supervisor for European Air Ambulance and an anaesthetist/intensivist emergency response physician, spoke to AirMed&Rescue about the ‘great progress’ that has been made with diagnostic capabilities in the prehospital stage of care. He explained: “An important diagnostic tool in clinical diagnostics is still the use of computed tomography and magnetic resonance imaging. These techniques make it possible to visualise pathological processes. For example, diseases in the thoracic region, such as lung parenchyma diseases, can be visualised.
“Pathological processes can be visualised in case of unclear craniocerebral diseases. Strokes can also be divided into ischemic and hemorrhagic strokes. This also has a direct influence on the therapy. With targeted diagnostics, we could thus already initiate a preclinical therapy.”
These diagnostic devices allow us to rapidly tailor blood product replacement to the individual patient, but until recently they have been bulky and fragile, limiting them to hospital use
LifeFlight Assistant Director of Education and Training Andrew Donohue was asked about what piece of diagnostic equipment is typically used in a hospital setting that can’t be taken onboard an aircraft. He responded: “It is tempting to say a CT scanner, since these give us so much information, but without access to surgery, it probably wouldn’t really change what we do. Rotational Thromboelastometry (ROTEM) and Thromboelastography (TEG) are variations of a technology that is becoming a key part of care for bleeding patients in the hospital setting. These diagnostic devices allow us to rapidly tailor blood product replacement to the individual patient, but until recently they have been bulky and fragile, limiting them to hospital use.” LifeFlight recently collaborated with Gold Coast University Hospital (GCUH) on a research trial, to prove that the latest versions of these devices could be used in the helicopter retrieval setting. The devices were tested using matched volunteer blood samples after being flown to GCUH on an RACQ LifeFlight Rescue helicopter and during a series of test flights.
“There is a growing understanding that major bleeding, especially due to trauma, causes a cascade of failures in the blood clotting system. TEG and ROTEM can rapidly pinpoint which clotting factors are deficient, allowing real-time optimisation of blood clotting, with the potential to reduce bleeding, minimise transfusion and improve patient outcomes. The GCUH and LifeFlight research showed that, while the devices don’t give accurate results in flight, they can be safely flown on an RACQ LifeFlight Rescue-operated AW139 helicopter. This shows the potential for this technology to be used to tailor blood product transfusion during preparation for aeromedical retrieval.”

Mobius Sp1
LifePort on Unique solutions for unique problems - sponsored content
LifePort develops and manufactures industry-leading medical interiors for fixed and rotor-wing aircraft. AirMed&Rescue spoke to Frank Graham, Vice President / Sales & Business Development, about the company’s processes, and its ability to provide tailored solutions to ensure products meet customers’ requirements and mission profiles.
The design/engineering influence can be driven by any number of contributors, explained Graham: “It may be that the operation requires a new medical mount to properly secure an new device for flight, it may be that the operator wants to add a capability to their mission like ECMO transports, or maybe the aircraft type is changing and an update to the certification is required.”
It is always the quickest and most cost-effective solution to utilize an existing product, but obviously this isn’t always possible in the world of aircraft special missions. Graham said: “Our philosophy is to deliver products and capabilities specific to the mission rather than trying to change the mission to because of the product. The alternative is that we utilize existing products and capabilities and change them to meet the new requirements and or augment the existing product with the new litters or mounts to give the customer what they want. Lastly, if a ‘tailored’ interior is preferred, we can accommodate this; we do totally unique tailored interiors a few times a year.”
When it comes to certification, thinking ahead is Lifeport’s strong suit, added Graham: “We overcome challenges by attempting to capture as many configurations as possible when completing the first approval. As an example, when we certify a new interior for a two-patient transport in an aircraft, we will typically add a configuration for a single patient as far forward in the cabin as possible and as far aft in the cabin as possible so that customers/operators have options. Additionally, we will also attempt to capture items that may not have be part of the initial contract, i.e. mission seats, monitor mounts, specialty litters, and redundant support equipment like compressed air pumps and inverters.”
Dr Simon Forrington, Medical Director of Capital Air Ambulance, agreed that radiological equipment such as chest X-rays and CT scans can’t be done on aircraft. There are also certain blood tests and other diagnostic tests that can be useful that are difficult to do onboard, especially in the current climate of Covid-19. Examples would be microbiological tests, including the diagnostic tests for Covid itself.
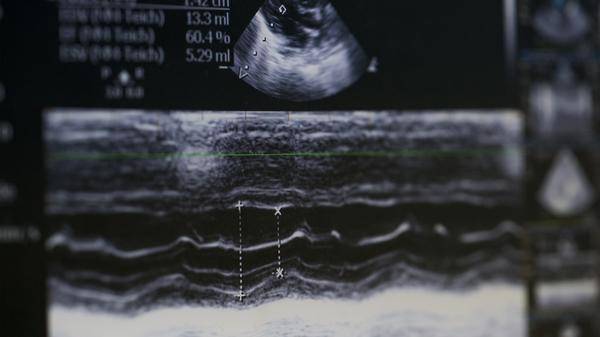
“It’s not really practical to do X-rays on the aircraft,” said Dr Forrington. “Some other blood and diagnostic tests can take several hours or even days to be organised and analysed / reported from the lab. Chest X-rays can reveal the presence of pneumothorax or pleural effusion (air or fluid between the lung and chest wall) which can be very dangerous in air ambulance flights. Happily, the recent availability of portable ultrasound scanning enables us to diagnose these problems instead of an X-ray.”
For Dr Adler, continued development of ultrasound devices – already vital – could further improve patient care through accurate diagnosis.
Examples of the kinds of tools already in use onboard air ambulances include portable ultrasound machines, some of which are so small that they plug into a mobile phone and use that screen to display the image from the patient. “The ultrasound,” said Sicard, “is a gold standard in emergency rooms around the world, and its use onboard air ambulances has led to drastic improvements in patient diagnosis.” The advances in sonography equipment are so important, in fact, that whether or not an air ambulance company carries one onboard their aircraft is one of the criteria that will allow that organisation to gain accreditation from EURAMI as a critical care medical transport provider.
Ultrasound is a gold standard in emergency rooms around the world, and its use onboard air ambulances has led to drastic improvements in patient diagnosis
Point of care laboratory equipment that allows a diagnosis such as a myocardial infarction (MI) is another game-changer. Again, used all the time in ERs around the world, technology such as stress radionuclide myocardial perfusion imaging or stress echocardiography, or cardiac marker analysis, to diagnose an MI in a patient being carried onboard an air ambulance can allow the doctor to decide on an immediate course of treatment, including asking the pilot to divert the aircraft if necessary. With the patient’s outcome being dependent on a fast diagnosis in such situations, air ambulances that can carry such testing equipment are in a strong position to improve patient care.

Butterfly IQ scanner
Just before Christmas 2019, medics working for the UK’s Great North Air Ambulance Service (GNAAS) were excited to welcome their newest piece of equipment – a Butterfly scanner (pictured above). Paramedic Lee Salmon explained the difference the scanner would make: “At the moment, we use a more expensive, less robust and comparatively older generation of ultrasound scanner. Although this older piece of equipment offers a degree of insight into a patient’s ‘hidden’ condition, the new Butterfly scanner is a brand-new piece of technology which has been put through its paces and it has been proven to offer a better clinical insight into a patient’s condition.
“When we use this on a patient, ultra-high sound waves are sent deep into their tissues and the way in which these waves bounce back essentially paints a picture of what injuries they have, and we can interpret this picture and formulate a plan of clinical care.”
The Butterfly’s ultrasound technology is an advancement on the traditional ultrasound, which allows medics to alter the software to suit the body region and vessels they are looking for. This kit costs in the region of £2,000 for the scanner; it then connects to an iPad mini – another cost – and then there’s an annual licence on the software of £1,000.
When we use this on a patient, ultra-high sound waves are sent deep into their tissues and the way in which these waves bounce back essentially paints a picture of what injuries they have, and we can interpret this picture and formulate a plan of clinical care
Salmon believes that this piece of equipment can mean the difference between life and death: “Identifying a cardiac tamponade (a build-up of fluid in the space between the heart and its sac) is essentially like identifying a ticking bomb that could go off in one minute or 30 seconds. We have already had one survivor due to the correct identification of a conscious patient who had a cardiac tamponade. He had open-heart surgery which was done by me and another doctor. The patient is now out of hospital and back at home.”
Portable Medical Isolation Units (PMIUs)
The Covid-19 pandemic has wrought havoc on almost every industry in the world, but air medical transportation couldn’t just stop – and, in many cases, companies are reporting that they are busier than ever. Portable medical isolation units (PIMUs) are not new, but Covid-19 has meant that the number of them being used to transport patients between hospitals and around the world has increased dramatically.
EpiGuard’s EpiShuttle solution has been particularly popular in Europe. Germany’s FAI was quick off the mark in February 2020, investing in several PIMUs. A spokesman for the company said at the time: “We installed a customised stretcher configuration on a Challenger CL604 aircraft, with specific EpiShuttle equipment and accessory modules ready to deploy. We have deployed a dedicated team of four ICU flight doctors and eight flight paramedics, now trained in accordance with the ECDC European Center for Disease Control Technical Directive: Infection Prevention and Control for the Care of Patients with 2019-nCoV in Healthcare Settings, February 2020.”
FAI enlisted the support of all its 70-strong team of pilots to perform duties. The biggest challenge remains scheduling, given the entry restrictions still in place in many countries around the world, many of which are not allowing entry for crew rest and pre-positioning.
Kenya’s AMREF Flying Doctors acquired two IsoArk Portable Isolation Chambers to respond to numerous requests to transport infected patients within Kenya and in the region. Dr Joseph Lelo commented: “The IsoArk N36-6 Portable Isolation Chamber from Beind industries in Israel was picked because of its weight, flexibility, ease of use and dimensions that fit our aircraft. The delivery timelines were also fast, and it has a good range of accessories and spares. The isolation chambers are also compatible with our Pilatus PC-12 fleet and our long-range jet air ambulance – the Cessna Citation XLS. This allows for transfers of Covid-19-infected patients from remote locations on unpaved airstrips in the East and Central Africa region as well as for long-distance transfers within Africa, and to Europe and the Middle East.”
Florida-based REVA Inc. invested in the ISOVAC CAPSULS unit for their infectious patients transfers. Steve Williams, Director of Global Air Medical Operations, REVA Inc., told AirMed&Rescue: “We are very pleased with our ISOVAC CAPSULS unit. It has enabled us to conduct long-distance, complex transports for patients who are confirmed or suspected of having Covid-19. It is an easy to use unit and so it has enabled us to quickly train our staff to use it.”
Current challenges for all aeromedical providers, said Sicard, include how to disinfect any equipment carried onboard. Cleaning the equipment used on patients needs to be cleaned after use, which can be time consuming and difficult.
Capital Air Ambulance also uses the Butterfly IQ scanner, and Dr Forrington noted: “We use the Butterfly IQ scanner, which displays the ultrasound image on our mission iPad. We can then quickly diagnose and treat conditions such as pneumothorax in real time, greatly improving patient safety on missions. The ultrasound can also be used to diagnose cardiac problems and fluid status when in skilled hands. They can be used to identify nerves when treating pain issues with a ‘nerve block’ and make this procedure safer and more likely to be successful.”
Ultrasound, then, can provide many diagnostic possibilities today, and since such devices are getting smaller and better, they can be used to good effect in aircraft. In these cases, they can at least partially replace the above-mentioned measures such as computer tomography and magnetic resonance tomography. However, they are not perfect, as Dr Adler pointed out: “The important distinction between ischemic and hemorrhagic stroke cannot (yet) be made by ultrasound devices. If we had such a diagnostic tool onboard, we could make the diagnosis earlier. In the case of an ischemic stroke, we could administer blood-thinning substances pre-clinically, which would be fatal in the case of a hemorrhagic stroke.”

In 2019, the HOVER (Handover of Ventilated Helicopter Emergency Medical Service patients in the emergency room) online survey was conducted amongst air rescue organisations in Germany, Austria, Switzerland, Italy and Luxemburg. The objective was to determine how many of them used the helicopter transport ventilator while transferring the patient from the landing pad into the clinic. In a secondary analysis, the authors looked at which factors influenced this use of the transport ventilator. Information gathered in the survey included which make and model of ventilator they used. In helicopters used for both rescue services and intensive care transport, the HAMILTON-T1 was ranked almost equally with the Dräger Oxylog® (2000plus, 3000, 3000plus).
In January of this year, WEINMANN Emergency launched MEDUVENT Standard, one of the smallest turbine-driven ventilators in the world. The device features turbine technology that maintains ventilation even without an external oxygen supply, and its manual mode is a new ergonomic and effective form of manual ventilation. Tidal volumes are defined by the MEDUtrigger and applied in combination with a pressure limit, which reduces the risk of hyperventilation as well as gastric insufflation compared to bag mask ventilation, while additional oxygen can be supplied to the patient at any time. The concentration can be adjusted flexibly from 21 to 100 per cent. Oxygen is supplied through a simple inhalation tube – thus ensuring worldwide compatibility and the patient’s oxygen supply.

TEMPUS-ALS device
In late 2019, the UK’s Air Ambulance Kent Surrey Sussex (AAKSS) equipped all of its emergency service helicopters with the Philips RDT Tempus ALS and Philips IntelliSpace Corsium web-based software platform. The collaboration with Philips RDT and AAKSS in the UK marks the first time anywhere in the world that Helicopter Emergency Service (HEMS) teams, which include a doctor and paramedic, can live stream patient medical information – including electrocardiogram (ECG), body temperature, heart rhythm, pulse and respiration rate and blood pressure – from the scene to the receiving hospital, as well as the on-call air ambulance team. Philips Enhanced Data Service (EDS) minimises data packets to enhance reliability over low bandwidth, preventing data loss during transmission. “This collaboration recognises our position as one of the world’s leading air ambulance services, bringing the most sophisticated technology to support the highly skilled medical teams we deploy across Kent, Surrey and Sussex,” said David Welch, Chief Executive Officer of AAKSS. “This will have a very significant impact in helping us to save lives and improve patient outcomes across the south east. With AAKSS demonstrating its application in real-life situations, we are confident the technology will be adopted by other air ambulances and partners in the health service.”
This will have a very significant impact in helping us to save lives and improve patient outcomes
Dr Joseph Lelo, Medical Director for Kenya-based AMREF Flying Doctors, said that recently, AMREF had acquired Zoll X series monitors. Lelo told AirMed&Rescue that these ‘robust and compact fully featured monitors that put advanced intensive care monitoring capability in a small package’ can be used for transport: “This monitor is very light, it has a multi-colour display that is easy to read. The X-series has the same capabilities as the E-series (pacing, monitoring, defibrillating) but can also perform invasive temperature and arterial pressure monitoring. The X-series is both Bluetooth and Wi-Fi capable.”

ROTEM machine
Medical device manufacturers that work closely with air medical providers are opening up a vast array of possibilities to improve and fine tune their products, as EAA’s Dr Adler explained: “We stay in close contact with the manufacturers, we give them regular feedback on the utilisation of their equipment in our aircraft and give them our ‘wish list’ for improvements of their existing equipment and development of new features.”
LifeFlight’s Andrew Donohue said: “I have not been involved in the final adaptation of equipment, but I worked with the manufacturers of the TEG and ROTEM devices in preparation for the discussed research. It was great to see how keen they were to be involved and the way prehospital and retrieval medicine is now being seen as a crucial part of medical care.”
Dr Forrington and the team at Capital worked with Butterfly IQ in testing the scanner in a flight environment, and with an unnamed company looking at cardiac output monitoring based on a patient’s pulse. He explained: “Specifically, whether the readings change significantly under the forces of acceleration and deceleration experienced in our aircraft. Finally, we are currently doing a study on EVDs (extra-ventricular drains – a device used to monitor and treat the pressure in the brain) and how they behave at altitude and during take-off and landing.”

EpiShuttle on PLUS with Mission Seats
Equipment that allows medical crews to manage blood products is a growth area, Sicard told AirMed&Rescue: “Carrying blood products is an increasingly important area for fixed-wing air ambulance operators carrying out critical care long-range transports, but sourcing [such] products can be difficult in terms of ensuring their quality and availability. For long-range critical care missions, air ambulance companies that can carry blood are in a good position in the marketplace.” Sicard also pointed to the potential for air ambulances to start carrying freeze-dried plasma, as is frequently the case in the military for combat medicine.
The GNAAS has already invested in a Mequ Blood Warmer, which can warm up blood from cold to body temperature in a few seconds, making it safe to give to the patient and prevent hypothermia. Holly Tayler, PR and Media Officer for GNAAS, said: “The lightweight warmer reduces the amount of equipment needed in the air, yet still has the capacity to warm cold blood on a single charge of the power pack. The warming of blood is essential on each flight – it’s that that saves lives.”
Under trial with the GNAAS earlier in 2020 was a sight-saving medical device that reverses the effect of chemicals on the body. Taylor explained: “If a patient had suffered burns to the eyes and body, this agent could prevent the person from going blind. With a chemical burn, the damage doesn’t stop, it will just continue to penetrate deeper into the tissue. This agent will help to stop that process. This specific agent is called Diphoterine ® solution. It is administered in a fluid form which is then irrigated over the patient’s eyes or the area of the burns.”
Artificial intelligence in healthcare is evolving quickly and will play an increasingly major role in diagnostics, in treating patients and in keeping people out of hospital in the first place
Capital’s Dr Forrington believes that the development of more portable – and more accurate – monitoring devices has improved dramatically, and changed patient outcomes with enhanced resilience in the flight environment and greater control for physicians. He added: “Coming soon, will be the ability to monitor patients fully remotely – i.e. the team at base will be able to see what is happening with a patient’s observations during flight and be able to offer advice in real time and treat problems before they arise. Wearable technology will also evolve, offering patient monitoring without the need for wires and heavy monitors that can be dropped and damaged. Artificial intelligence in healthcare is evolving quickly and will play an increasingly major role in diagnostics, in treating patients and in keeping people out of hospital in the first place.”
Donohue agrees: “A key advancement I expect in the future is greater integration between devices and much better collection of data. I think when we arrive at a hospital, in the near future, they will have already received a secure transmission of the complete digital record of the whole mission, including scene photos, continually updated vital signs and ultrasound images.
“One of the most exciting things for me is that, considering 10 years ago we didn't carry portable ultrasound devices and wouldn't have even imagined using TEG or ROTEM in retrieval, we'll probably have equipment we haven't even thought of yet.”
A brave new world awaits for medical equipment device manufacturers!
August 2020
Issue
- Air ambulance medical equipment innovation and development
- Introducing a safety culture in HEMS
- Provider Profile: LifeFlight
- Air Ambulance Worldwide discusses the fallout of Covid-19
Mandy Langfield
Mandy Langfield is Director of Publishing for Voyageur Publishing & Events. She was Editor of AirMed&Rescue from December 2017 until April 2021. Her favourite helicopter is the Chinook, having grown up near an RAF training ground!


