Neonatal transportation in the west of the USA

Amy Gallagher provides a comprehensive look at the clinical issues of neonatal transportation as shared by the experts: NICU transport nurses in the ‘Wild West’
Although specialty neonatal care reduces rates of air medical transport, nearly 70,000 neonatal transports still occur in the US annually. Calming the ‘perfect storm’ of neonatal air medical transport while managing the tiny details before, during and after the transport, neonatal teams must be well-equipped and highly trained to calculate the risks. With the fortification from the most innovative equipment, advanced technology, and extensive knowledge from the latest research ensures safe deliveries of their tiny parcels, the neonates.
North central Texas: Right skills, right equipment at the right time
Efficiently managing the limitations and effects of the transport environment on the neonate patient demands attention to the tiniest of details and specialized expertise – notably in remote areas, where the right equipment is on standby and the right skills are at the ready for when the weather can be anything but friendly.
Like the ‘perfect storm’ that seems to be the norm in the neonate transport, the term ‘remote’ is often defined by the very essence of the details required for the neonate. “[There is] the luxury of experts on standby for all healthcare emergencies, but it never fails: the sickest babies are born in remote areas during the worse weather,” said Stacy Putman, Director of Transport, Teddy Bear Transport Team, Cook Children’s Medical Center, Fort Worth, Texas. “We are fortunate in Texas for the specialized neonatal transport teams who deliver a high level of expertise.”
But in Texas where ‘everything is big,’ it could be ‘many hours before a specialty team arrives on scene,’ Putman said. Texas boasts 268,596 square miles creating a huge dynamic, but there is no dynamic too big for the smallest of transport patients.
With the Teddy Bear Transport’s aerial assets of a Citation Encore+, King Air 200 and EC145, Putman said the pilots, mechanics and certificates provided by Metro Aviation are key in remote areas.
“But not all teams carry the same equipment,” Putman added. “Standard equipment includes an incubator with a conventional ventilator and possibly high frequency ventilation (HFV), while the more advanced teams deliver nitric oxide, active cooling and transfer on the extracorporeal membrane oxygenation (ECMO) system.”
Standard equipment includes an incubator with a conventional ventilator and possibly HFV, while the more advanced teams deliver nitric oxide, active cooling and transfer on the ECMO system
The logistics of securing the extra equipment, such as the advanced technology in the ECMO, is designed to prevent respiratory failure, but represents the biggest hurdle of transport that requires the intentional and methodical transfer into, and out of, the transport isolette.
“Even the slightest tug on the ECMO catheters could dislodge them from the neonate’s extremely small veins and arteries,” said Putman. “The Hamilton T1 is great for conventional ventilation with its diverse non-invasive and invasive modes, and the TXP for HFV and the TECOtherm NEO for active cooling.”
The absence of market competition in the neonatal product development space is also a big dynamic. Looking forward to the next generation of incubators, mobile transport options for neonates and research-based treatment protocols, Putman complimented International BioMed’s newest incubator ‘which has done a great job of streamlining a lot of equipment into one high-tech incubator.’
“However, the evolution of the neonatal product development overall market is slow in coming,” explained Putman. “Nitric delivery options are very limited. The addition of fresh ideas from other developers would be welcomed.”
“Currently, the market has only one option for active cooling in the TECOtherm NEO,” said Putman, which is an innovative active cooling device for whole-body active cooling and warming for mobile therapeutic hypothermia needs. “Our ability to do all these treatments is the ‘gold’ standard,” she said.
The golden moment for the Teddy Bear Transport team was in celebrating 40 years of service last year. “We heard hundreds of stories as we celebrated this milestone.
“Many of our patients are now parents themselves. … It’s best job ever,” she concluded.

Multi-state southwest US: Low birth weights in the high country
Further to the northwest of Texas is the University of Utah’s AirMed neonatal transport team with one respiratory therapist and two neonatal intensive care unit (NICU) nurses, including Melanie Thelin, who is prepared if ‘an initial call comes in for maternal, knowing it can quickly turn into a NICU delivery.’
“Working in both the NICU and transport provides the vision of detailed pathways of neonatal care,” Thelin said. “Exclusively used for NICU transport, the EC145 twin engine provides enough space for obstetric transports in the event of a delivery and for all of the equipment from the NICU.”
One of the changing dynamics in neonate transport is the low birth weight of neonates, which requires diverse sizes of equipment.
“It’s not a ‘one size fits all’,” she explained. “Our isolettes are customizable with at least one ventilator as a standard, and the use of an HFV. Neonates weighing 400g with fragile lungs may not tolerate conventional ventilators, which is when we use a second ventilator with HFV.”
Utah’s AirMed Team ‘gold standard’ currently uses heated isolettes to ensure the baby’s temperature remains stable during transport.
“For ‘premies’ who require a higher level of care, we completely stabilize the neonate prior to take off,” said Thelin. “It’s our team’s ‘hands off’ goal, knowing it’s already a stressful time for the baby.”
In the future, the team would like a more soundproof single-walled isolette and a probe with detailed definition to see the ‘lung fills’ for the placement of umbilical lines without an X-ray.
“Although we have an ultrasound on the baby’s lungs to neo aspirate in the air, we can’t listen with a stethoscope as the air deteriorates,” Thelin explained.
Preparing for all the ‘air-to-mountains’ dynamics during the ‘summer and winter survivals’ requires the details of highly specialized training to transport neonates in one of the largest, and most unique, geographical areas of any flight program in the nation; representing Utah, Colorado, Wyoming, New Mexico, Nevada, Montana, Idaho and half of Arizona.
Pediatric cardiologists on staff provide instruction on cardiac congenital anomalies explaining the various treatment protocols
As a higher educational institution, the university’s AirMed team benefits from the available resources built within the university including a full-time neonatologist, who conducts research devoted to Utah, quarterly educational sessions, simulation training, and annual training conferences held within the school and organized by the team.
“Pediatric cardiologists on staff provide instruction on cardiac congenital anomalies explaining the various treatment protocols,” said Thelin, who explained that the university has the highest birth rates of cardiac patients in the nation.
In the meantime, the team is finding joy in the big gatherings of their smallest patients; the team enjoys providing follow-up care for all their neonates throughout their development as a standard of care.
“One of our greatest joys as a team is the university’s AirMed annual reunion when we welcome all our NICU ‘graduates’ with their parents, who are always so grateful,” said Thelin.
Northern Arizona: Investing in expertise and technology
Based in Flagstaff, Arizona, the Northern Arizona (NA) Healthcare’s Guardian Air (GA) transport team is always on standby. As Chief Flight Nurse and Clinical Manager, Ben Perry said: “We bring expertise to the bedside of the remote areas of NA with the most modern transport and equipment using temperature-controlled isolettes from International Biomed for our high-risk neonatal patients.”
The GA transport team includes one neonatal team lead RN, and an RN-trained or other specialty-trained paramedic certified through the state of Arizona to transport any age neonate. The only transport service in NA providing maternal and neonatal, GA transport flight department includes a Bell 407 helicopter and Pilatus PC-12 fixed-wing aircraft.
“Based on my research, our ‘gold standard’ for equipment is the latest isolette with a Zoll monitor, with end-tidal carbon dioxide (ETCO2) monitoring, arterial line monitoring, defibrillation and pacing,” said Scott Beckstead, Patient Specialty Coordinator, GA Transport. “For ventilation, it is a Hamilton T1 ventilator for traditional ventilation and a TXP HFV ventilator.”
Perry said, “For the future, we would like to have nitric oxide capabilities and instant blood gas monitoring, with built-in bilirubin lights, and an isolette with a ‘Servo mode’, not just a heater. “With the exception of nitric therapy, we are currently waiting on equipment to provide all of these capabilities on one of our isolettes.”
As a continuously accredited member of the Commission on Accreditation of Medical Transport Systems (CAMTS) since 1996, the GA transport team receives survival and air medical resource management (AMRM) training as well as daily safety topics, monthly safety meetings, conferences and educational sessions, and quarterly educational units via education modules presented by the NA Healthcare’s NICU nurse educators while discussing research from its neonatal nurse practitioner (NNP) and neonatologist.

East Texas: Warmed and humidified gases
“With the uptick in neonatal and pediatric respiratory illnesses in transport in recent months, we have maintained a strong focus on heated, humidified oxygenation to prevent mucous plugging and to maintain optimal ciliary function in the airways,” said Dawn Johnston, Administrative Director, Nursing and Clinical Services, CHRISTUS Flight For Life. “The tiny cilia ‘hairs’ beat rapidly to move mucus and particulates up and out of the respiratory system, but without warmed humidification they quickly dry up and stop working. Without oxygenation that is heated and humidified, we could worsen their airway situation and even lower core temperature.”
We have maintained a strong focus on heated, humidified oxygenation
“High-flow nasal cannula therapies (HFNC) have been an effective tool for transport of spontaneously breathing patients and this remains an important part of our ongoing training,” she added. “In addition to our standard ventilator training, the team has had good success using the Airvo 2 in transport,” Johnston said. “It’s designed to heat and humidify the oxygen and other cold, dry medical gases, and has worked very well for our spontaneously breathing patients.”
In recent years, Johnston said that the staff was also provided the option to earn their Neonatal Pediatric Transport Subspecialty certification (C-NPT): a two-day prep course that includes the team’s respiratory therapists, advanced practice providers and physicians.
“The purpose of the C-NPT is to provide a competency-based examination that tests specialty knowledge and the application of that knowledge for licensed healthcare professionals in the US and Canada who provide stabilization and transport interventions to critically-ill neonatal and pediatric patients in all types of settings,” she explained.
Conclusion
Being able to attend to the care of unwell and critically-ill infants within the austere environment of neonatal aerial transport requires the latest research, innovative technology and the most advanced equipment in the marketplace. There are also requirements for annual and quarterly training through simulation; collaborative conferences; daily reviews of the latest research; specialized certifications; and aerial assets in rotor- and fixed-wing aircraft. These are needed to navigate the most demanding situations during unpredictable weather scenarios to safely transport the tiniest of patients – neonates – who depend on the most qualified neonatal transport teams in remote and rural US to manage even the tiniest of details to ensure the best of outcomes.
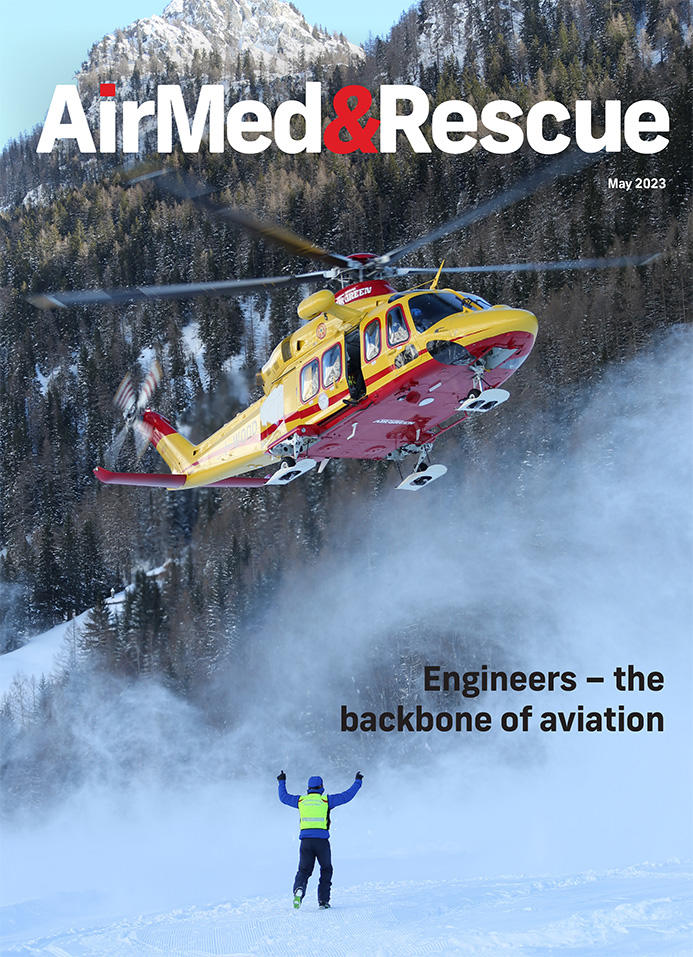
May 2023
Issue
We speak to engineers about their work; we find out about the demands for transporting neonates; we explore when VLATs are the superior choice for firefighting; we look at the tools and training to ensure positive outcomes in the event of a power failure; plus all of our regular content.
Amy Gallagher
Amy Gallagher is an internationally published journalist covering aviation, rescue, medical and military topics, including evidence-based research articles. As a journalist by education and certified English instructor, Amy has worked in both agency and corporate communications, providing educational and promotional writing and training services through her agency, ARMcomm Writing & Training, www.ARMcomm.net.


