Interview: Gretchen J Carrougher, Research Nurse Supervisor for the University of Washington (UW) Medicine Regional Burn Center

A team effort: Mandy Langfield talks to Gretchen J Carrougher, Research Nurse Supervisor and Chair of BCEN CBRN ECRC, about her career in burn nursing
What’s your clinical background and experience, and how have you progressed to your current role?
My nursing career began at the MedStar Washington Hospital Center in Washington, DC. As a graduate nurse in the burn intensive care unit, I began this journey by learning how best to care for those impacted by burn injury. From there, I’ve worked at two other burn centers – the US Army Institute of Surgical Research (also known as the Army Burn Center) and UW Medicine Regional Burn Center, where I’m a Research Nurse Supervisor. Throughout my 41-year career, I have been mentored and educated as a clinical nurse specialist and now as a researcher.
What do you enjoy most about your current role?
I am Research Coordinator for the Northwest Regional Burn Model System, which is grant-funded by the National Institute on Disability, Independent Living, and Rehabilitation Research. The focus of our studies is on the rehab and community participation of those impacted by burn injury. I enjoy both the survivor and family member contact with our studies, but also the ability to share research findings with others at the bedside – whether they are nurses, surgeons or the carers. Burn teams have existed for many years, and we have demonstrated that the team approach to care is critical to the successful recovery and community reintegration of survivors.
You have just accepted the volunteer position of Board of Certification for Emergency Nursing’s (BCEN) CBRN Exam Construction Review Committee (ECRC) Chair – what does this involve?
For many years, the burn care community has advocated for a national burn nursing specialty certification. Following the official recognition of burn nursing as a specialty in 2020 by the American Nurses Association, the American Burn Association approached BCEN to develop a burn nursing specialty credential. BCEN began that work in earnest in summer 2021, the first burn nursing role delineation study was completed in spring 2022, and the Certified Burn Registered Nurse (CBRN) exam content outline was published in fall 2022.
In my role as Chair of BCEN’s CBRN ECRC, I work with a small team of nurse volunteers – both burn nurse and exam-writing experts from trauma. We are meeting virtually to review and finalize the CBRN exam questions. The inaugural CBRN exam items have been developed by a larger and dedicated group of burn nurses who received special training in exam item writing. There is a very intentional emphasis on making sure that the composition of the nurses involved with the certification program represent our community in terms of geographic, demographic and practice diversity, plus educational preparation. In the longer term, the BCEN ECRC is responsible for ensuring that the CBRN exam accurately and fully reflects the scope and practice of burn nursing – including roles, current clinical knowledge and professional issues. It is an honor to be a part of this historic advancement in our specialty.
Trauma patients with burns are often transported by air ambulance to the nearest burn care center. What advice would you give to paramedics and flight nurses?
I believe that the Advanced Burn Life Support Course (ABLS) is an excellent resource for both paramedics and flight nurses. ABLS provides critical knowledge for the immediate care of the burn patient during the first 24 hours following injury, including transportation. It is available live, with didactic lectures and hands-on simulations, as well as an online, self-paced course. It also provides information on mass casualty preparedness and was updated in January 2023.
Additionally, some flight nurses may look to become certified as a CBRN. This advanced certification is an especially good fit for registered nurses working at burn centers and units, because it spans the entire scope of burn nursing – from prehospital and acute care through to rehabilitation and reintegration, also offering an opportunity for transport nurses who would like to expand and validate their knowledge.

What are the latest developments in treatment that first responders are being trained in?
In the past several years, information on early fluid resuscitation measures for the patient with a significant burn injury were revised. No longer do we simply say: ‘Place two large bore-IVs and begin fluid administration.’ Today, during the primary survey, patients who will likely need intravenous (IV) fluid resuscitation (e.g. those with burns of more than 20 per cent of their body surface area) receive it based on their age. This is easily identified, thus making the on-site/prehospital fluid administration easier to provide. Once the size of the burn injury has been estimated, which occurs during secondary survey, the fluid rate is adjusted based on a formula, then further titrated based on patient response (which is typically the patient’s urine output). This change in practice will hopefully ensure that adequate fluid resuscitation volumes are administered prehospital, such that both under- and over-resuscitation are avoided.
The recommendations for referral to a recognized burn center have also been revised. The Guidelines for Burn Patient Referral now include information on what the American Burn Association recommends for immediate consultation, with consideration for transfer versus consultation alone. These new guidelines differ from the previous recommendations that only listed injuries that required transfer to a burn center.
What equipment must be carried onboard a HEMS aircraft to provide appropriate care?
Although I have not had the opportunity to provide burn care in-flight, it’s my understanding that critical care HEMS aircraft carry all the equipment and supplies – including a cardiac monitor, ventilator, IV fluids and numerous medications – necessary to provide burn care, similar to what you would find in an intensive care unit. The Commission on Accreditation of Medical Transport Systems has an extensive list of onboard equipment and supply requirements for critical care transport, as does each state.
Besides the benefit of rapid travel to an appropriate facility, it is really the training of the onboard personnel that benefits the burn patient. Transport of a critically injured individual, especially during the first 48 to 72 hours after injury, can be difficult. Understanding the pathophysiology of injury as it relates to thermoregulation and burn shock during this early time period are critical.
What can civilian HEMS operators learn from the military’s approach to burn care?
I have worked at the USAISR, the Army’s Burn Center in San Antonio, and witnessed first-hand its capability to care for the critically injured burn patient. As I said, I am not a flight nurse, but clearly the US Army burn flight team’s years of experience, beginning in the 1950s, has led to improved outcomes for those who require long-distance transport. Issues to consider – and should be part of best practice – are the needs of the patient; the capabilities of the facility currently caring for the patient; the likelihood of deterioration during transport; the ability of the transporting team to deal with such deteriorations; and the benefit to the patient of transporting them to a location where definitive care can be provided (in other words, a burn center). As we consider each of these factors, we must remember that burn patients can be very unstable during the first 24 to 48 hours after a major injury, and that errors in resuscitation can occur and have consequences that may result in complications. Managing burn shock during a long-range air transport may be difficult, even for the most experienced provider.
These patients are also going to have mental trauma; what specific care is needed for that?
As a specialized care team, we are aware of the emotional trauma that individuals and family members often experience. Burn teams in the US have psychologists and/or psychiatrists, who can see patients soon after admission to help with personal recovery. Burn nurses are astute at screening for acute and post-traumatic stress, and aware of common emotional issues and concerns that evolve after injury. Many burn centers in the country participate in the Phoenix Society for Burn Survivors SOAR (Survivors Offering Assistance in Recovery) program. This connects survivors and loved ones with others who have experienced similar trauma (a kind of peer support). Collectively, burn centers provide a holistic approach to recovery, which includes treatment that addresses both physical and mental health concerns.

Is the US suffering from a lack of burn care centers of excellence, and as rural facilities face more closures, what does this mean for patients? Does it make HEMS transport even more vital?
Good question. There are many US burn centers that provide excellent, evidence-based care. However, there is not always one within ‘miles’, particularly in more rural areas. For example, I work out of Harborview Medical Center in Seattle, Washington, and we serve a four-state region including Alaska, representing about 24 per cent of the land mass of the US. Thus, we must work closely with those we serve in our catchment area, including transport teams who may have to travel with a critical burn patient for hours before reaching definitive care. Communication and coordination are key to effective practice and optimal patient outcomes – and it is essential to include our transport colleagues.
Gretchen Carrougher
Gretchen Carrougher, MN, RN, is a Research Nurse Supervisor at the University of Washington Medicine Regional Burn Center at Harborview Medical Center, and Program Coordinator for the Northwest Regional Burn Model System. Gretchen has been a staff nurse, clinical nurse specialist, outreach educator and research nurse in burn care for over 40 years.
March 2023
Issue
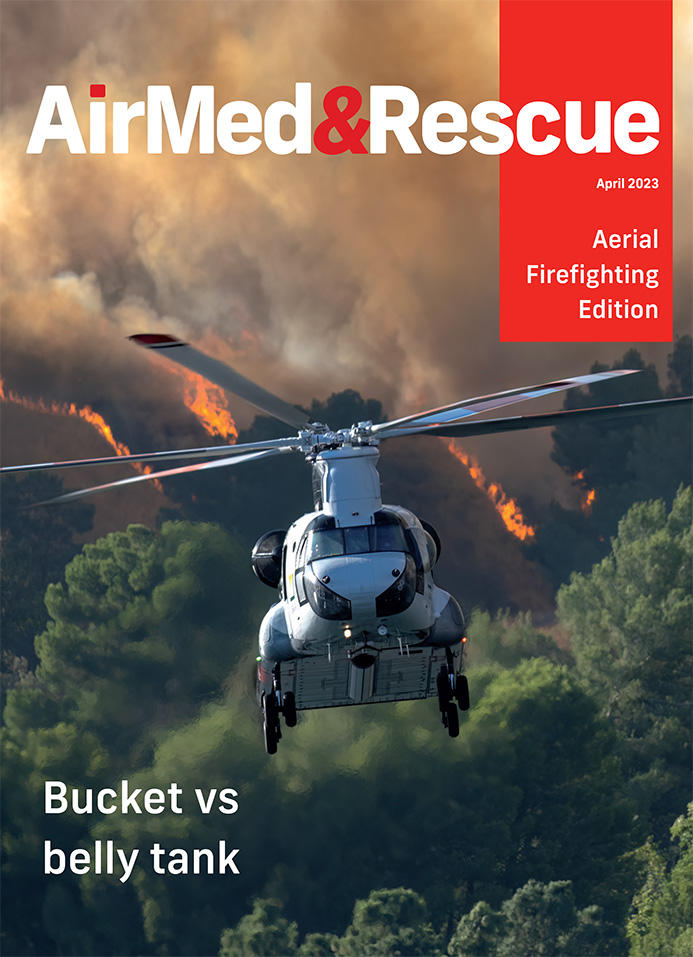
In the April 2023 aerial firefighting special issue
When preparing for a fire season, what are your choices for the type of fleet contracts you will use; location, situation, capacity, and a multitude of other considerations need to be made when deciding whether it is best to use a belly tank or a bucket, and what is the alternative; data collection and analysis have become more and more important when managing an attack on a wildfire, what software and equipment is available, and how can you manage integration and communication to improve your effectiveness in fighting fires; plus a whole lot more to keep you in the loop and in the air.
Mandy Langfield
Mandy Langfield is Director of Publishing for Voyageur Publishing & Events. She was Editor of AirMed&Rescue from December 2017 until April 2021. Her favourite helicopter is the Chinook, having grown up near an RAF training ground!


