Interview: Dr Andy Lockyer, Medical Director for Great Western Air Ambulance Charity

High performance and cutting-edge care: Dr Andy Lockyer tells Jon Adams why PHEM is more rewarding than running onto a sports stadium
What new challenges have you as the Medical Director of GWAAC faced since you stepped up in July, and do you find you still have time to personally work shifts in critical care for GWAAC as before?
Naturally, one of the greatest opportunities and challenges of leading a clinical team like GWAAC is that it is a small
I strongly believe if you give excellent people the right conditions, they naturally achieve excellent things for their patients
team of exceptionally skilled and experienced clinicians. It means the team is capable of really high performance and developing cutting-edge care. This does mean managing to bring together all that experience and knowledge in a way that the team all supports and gets behind. While we have a clear vision for what the team wants to achieve, I strongly believe if you give excellent people the right conditions, they naturally achieve excellent things for their patients.
What aircraft does GWAAC operate and how is it equipped and crewed?
We fly an EC135. The entire aviation operation is provided by Babcock but we’re lucky to have two full-time base pilots who work really closely as part of our team. We would be normally crewed with a pilot, a specialist paramedic in the role of technical crew member, a doctor, and often a fourth person in a training role. Our pilots are superb at supporting us with logistics and practical tasks on scene with patients while handling the safe transport of crew and patients at all times.

Your aircraft is only operated during daylight hours, with your fleet of cars helping to cover the late, after nightfall, shifts. Are you exploring night flight operations, and what considerations would that need?
We are lucky in our traditional geographical area, night driving on the excellent road network gets us to ‘after dark‘ jobs in a way that would generally be quicker than night flying with the processes inherent in night operations, but it’s something we always continue to review.
Our crew allows us to provide full critical care, as well as ‘enhanced care’ where specialist paramedics can still support ambulance crews with enhanced skills and treatments
There has been a rise in the number of incidents that air ambulance charities are responding to, year on year. How are GWAAC preparing to accommodate this growth going forward?
In order to best use charity funds to save lives, we take a very data-driven approach to our service. We aspire to providing 24-hour critical care in the near future but we want to balance setting up our service to reach the highest number of critically unwell patients, while also having the public rely on a quality of care that will be available to anyone on their worst day. Our crew allows us to provide full critical care, as well as ‘enhanced care’ where specialist paramedics can still support ambulance crews with enhanced skills and treatments. We need to know what kind of patients are leading to a rise in overall numbers so we can deploy the right teams to the right geographical areas to provide the right care. We also increasingly hope that different air ambulances can work together across traditional geographical boundaries to work collaboratively to reach patients and provide them the treatment they need.
In another of your capacities, you are heavily involved in global outreach of emergency care. How do other countries manage PHEM and what can we learn from your experiences abroad?
Pre-hospital care is hugely variable globally, and it’s very easy to take for granted here in the UK that we
I often thought we could learn a lot from how communities respond to emergencies, and the innovative informal system that develops to meet the emergency needs of local populations relatively effectively
have such a good pre-hospital care infrastructure linked into NHS care. It’s interesting when developing pre-hospital systems that similar European countries have often matured into very different systems. When I worked in low- and middle-income countries, I often thought we could learn a lot from how communities respond to emergencies, and the innovative informal system that develops to meet the emergency needs of local populations relatively effectively. I run a charity, Dharura: Global Emergency Care, and one of our projects is to provide rural rangers and community leaders first responder care and transfer to hospital.
GWAAC isn’t just a reactive charity, it has several training and education programs, for medical trainees, the general public and children. Can you explain a bit more about them?
GWAAC considers the whole ‘chain of survival’ for our most critically unwell patients, and tries to invest and engage at every step of this to get as many patients in our community the best outcome from their illness or injury. From supporting a community defibrillator program, training adults and children in cardiopulmonary resuscitation (CPR) and the use of these devices, to outreach education with ambulance crews around critical care and training alongside our hospital colleagues, GWAAC supports innovation and improvement at every stage of the patient journey, and we can have a role as champions for this.

GWAAC has met with an electric vertical takeoff and landing (eVTOL) aircraft manufacturer about the requirements for helicopter emergency medical services (HEMS). Do you think eVTOLs will be used for HEMS in the near future and is that a direction that GWAAC is exploring?
We are in the very early days of exploring the use of eVTOL aircraft but we will consider any opportunities that help us achieve our vision that everyone receives the lifesaving pre-hospital emergency care they need with as little impact on the environment as possible.
Are there any particular plans for 2024 for you or GWAAC?
While we continue to develop our service and care provision, we have a few things we really want to develop at GWAAC over the next year. We want to be increasingly outward-looking with more opportunities for observers and engagement with other services we work alongside. We’re also working really hard to address barriers to careers in pre-hospital care that will help improve diversity in our team, and ensure there is equality of access to PHEM careers. Pre-hospital services have dramatically changed over the last 10 years, and we’re really keen to ensure the professionalization and development of our service keeps GWAAC at the forefront of pre-hospital critical care.
We want to be increasingly outward-looking with more opportunities for observers and engagement with other services we work alongside
Some other goals include:
- Running a clinical symposium and building on our outreach work, including leveling the playing field to enable more women and ethnic minorities to access PHEM training
- Growing our Great Western Hearts program by securing 80 new defibrillator hosts and training 10,000 people in lifesaving CPR and use of a defibrillator, focusing on the people that need it most
- Opening eight new charity shops, helping us to generate a sustainable income in a way that is both environmentally friendly and supports local communities.
December 2023
Issue
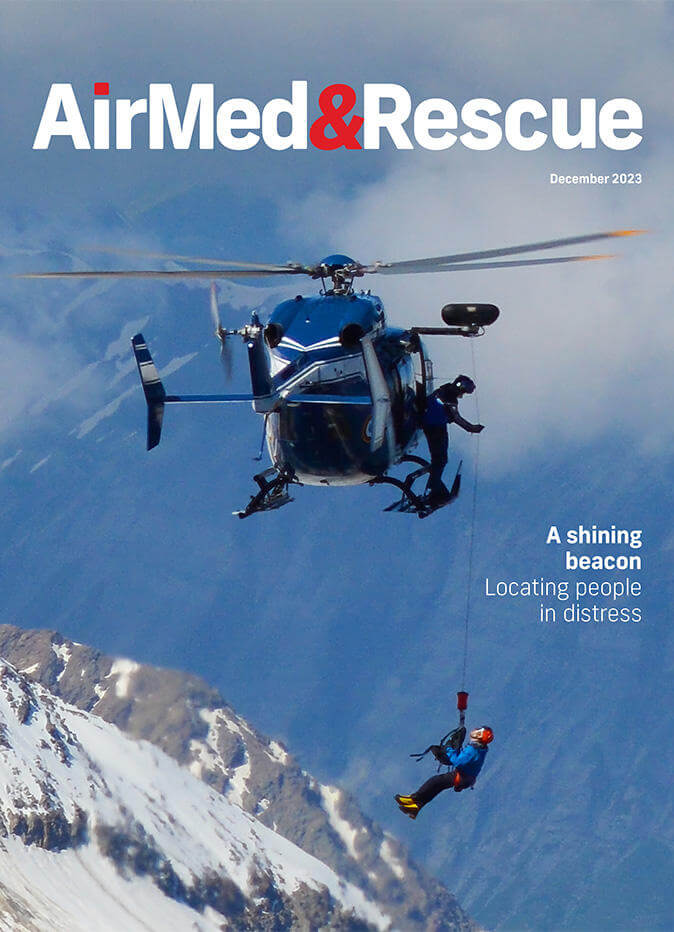
In the December edition, we cover personal locator beacons to aid with rescue; rescue operations in Mediterranean Sea; preparation for southern hemisphere fire seasons; and the value of sleep and rest for safe operations; plus more of our regular content.
Jon Adams
Jon is the Senior Editor of AirMed&Rescue. He was previously Editor for Clinical Medicine and Future Healthcare Journal at the Royal College of Physicians before coming to AirMed&Rescue in November 2022. His favorite helicopter is the Army Air Corps Lynx that he saw his father fly while growing up on Army bases.

