Innovations in critical care

Dr Joetey Attariwala spoke to military and civilian aeromedical care providers to find out which tools they are currently using in their arsenal to provide the best possible care to critical patients
The topic of innovations in critical care techniques as it pertains to outcomes for aeromedical patients is a broad one, the pulse of which lies squarely on the aeromedical professionals that render that care.
Team set up
The operating concept of aeromedical providers differs significantly between countries. For example, Helicopter Emergency Medical Service (HEMS) providers in the UK regularly respond with doctors as a part of the crew, whereas doctors are rarely part of HEMS teams in the US or Canada, with the exception of pre-planned flights necessitating a physician onboard. It therefore comes as no surprise that a crew consisting of a physician would be able to render a greater degree of critical care than those without.
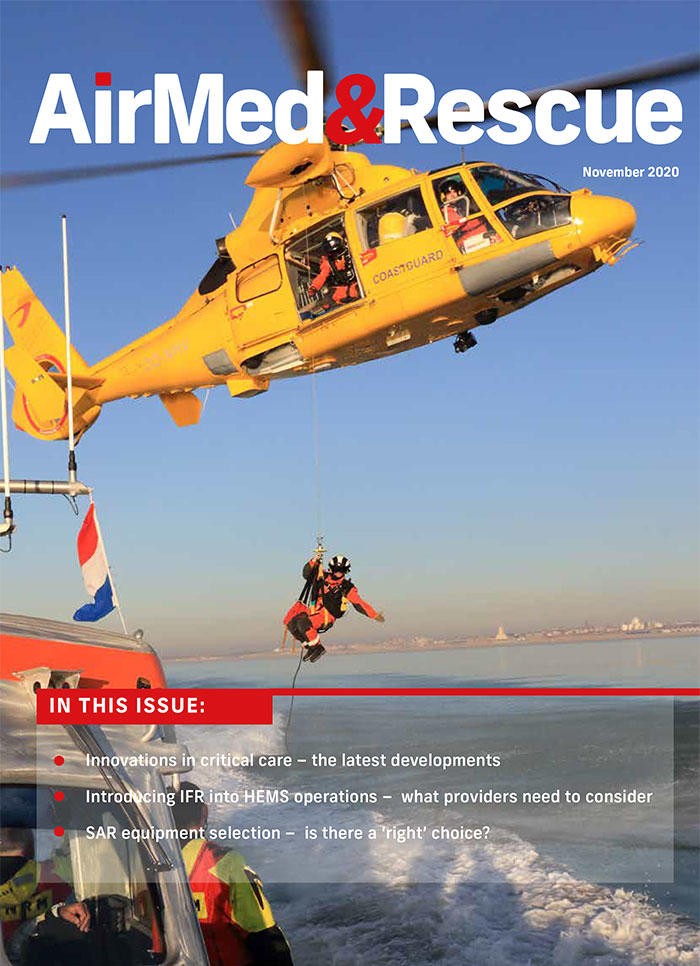
it is essential that aeromedical platforms are expediently and efficiently vectored to a scene, or to a location where search and rescue can be expedited
Many factors contribute to patient survival; in the case of emergency aeromedical care, the core fundamental of responding to incidents in a timely manner – preferably within an hour (often referred to as the golden hour) is as relevant today as it ever was. In this case, it is essential that aeromedical platforms are expediently and efficiently vectored to a scene, or to a location where search and rescue can be expedited.
Speaking to these points was David Olvera, Air Methods Director of Clinical Research: “Traditionally, the idea of transporting a patient was to urgently get them from point A to point B. With advancements in evidence-based practice and prehospital care, the use of a physician and nurse in HEMS or fixed-wing operations allows for improved treatment. Thus, modifying the way we transport patients from ‘a load and go process’ to an urgent medical transport resource offers advanced opportunities to stabilize or improve the patient’s outcomes.”
Effective communications plays a key role in all events, so the utilization of beyond line-of-sight and satellite communications is more important than ever; not only for air traffic control and communication with ground teams, but also for communications with medical centers, which can provide enhanced telemedicine support to aeromedical crews as and when necessary. This communication is typically verbal in nature, but there is also growing capability to transmit patient vitals and other medical information directly to emergency departments for assessment and guidance.
One aspect of aeromedical care that gets little attention is ride quality, whether it be rotary or fixed-wing platforms; this aspect of aeromedical transport is equally as important to aeromedical crews that are rendering aid as it is for patients, where smooth transit in temperature controlled aircraft is optimal (as is adequate pressurization at altitudes over 10,000 feet above sea level).
Aerospace physiology is widely understood, so advancements in this area to yield improved patient outcome is modest
Aerospace physiology is widely understood, so advancements in this area to yield improved patient outcome is modest.
With that said, Olvera believes advancements of evidence-based practice in HEMS and fixed-wing transport has improved patient care, because all entities are instructed in research-based information, which is proved to improve patient care and quality of life: “With the advancement of evidence-based critical care, medical transport patients are showing improved survival when transported to hospitals,” he explained.
“One example of this is combining the difficulties placed on maintaining airway management on a patient in the critical care air medical transport environment. Improved patient care is due to having a better understanding of gas laws and physiological outcomes of our patients while in transport. One specific example is looking at ventilation and oxygenation of our patients during transport and working on proven techniques that improve outcomes with the latest in ventilator technology,” continued Olvera.
“From a physiologic standpoint, the same issues are encountered in the intensive care unit (ICU) and emergency departments. Thus, the phrase has been coined ‘out of operating room airway management’. We have learned that we all have the same physiological issues with our patient care by combining forces with ICUs, emergency rooms and pre-hospital practices. This combined collaboration has allowed us to improve practice. Additionally, current literature and research from the prehospital setting are being implemented for studies in the hospital setting to help improve patient care.”
Infectious patient critical care transport
Two areas that continue to advance in critical care techniques are medical transport technology and training. The former has significantly evolved as military aeromedical units have focused attention on bio-containment technologies in the wake of the Ebola virus, and more recently for the Covid-19 pandemic.
Ebola and Covid-19 have renewed focus on infectious disease critical care transport. Governments have the most resources to mobilize to these situations, and that has led countries like Canada and the US to rapidly procure such capability in order to save lives.

Speaking to AirMed&Rescue was Lieutenant-General Al Meinzinger, Commander of the Royal Canadian Air Force (RCAF): “I often talk about agility as being one of the key characteristics of the Air Force – and that includes some rapid procurement work. We’ve fast tracked and are in the process of procuring some infectious disease mobility equipment that would allow us to medically transport patients in our aircraft in a safe manner. It’s been done with a great deal of priority due to Covid-19.”
Canada is executing on a series of emergency procurements to reduce the risk of contamination of medical teams, aircrew, and aircraft while transporting infected patients. Four procurements are currently underway: Aeromedical Bio-containment Evacuation System (ABES) is a specially designed large isolation unit, which fits in CC-130 Hercules and CC-177 Globemaster aircraft to provide a space where multiple infected patients can be kept and treated by medical staff while ensuring the safety of the aircraft’s crew during long domestic or trans-border flights.
The Aeromedical Single Isolation Bio-containment Unit (ASIBU) is a reusable hard-shell capsule that carries one patient and allows medical staff to provide advanced medical care during transportation
The Aeromedical Single Isolation Bio-containment Unit (ASIBU) is a reusable hard-shell capsule that carries one patient and allows medical staff to provide advanced medical care during transportation. Its hard shell provides safe operation in an aviation environment, including helicopter operations, and allows quick decontamination between missions. The Disposable Isolation Single Bio-containment Unit (DISBU) is a soft-shell lightweight unit that is quick to deploy and packable. They are suitable for isolating stable patients, improving aircrew safety over short distances. And finally, the Griffon Helicopter COVID Barriers are meant to separate pilots in the cockpit of the Griffon helicopter from the passengers in the cabin, and will serve as a complement to other protective measures.
“The RCAF is on the path to becoming much more agile in the safe aeromedical evacuation of infected patients. Over the next six months, emergency procurements totaling $7.3 million will provide the RCAF with the most advanced equipment commercially available to build a capability for now and for years to come,” said Meinzinger.

The US Air Force Air Mobility Command (AMC) is also rapidly fielding and positioning an infectious disease critical care transport capability. The Transport Isolation System (TIS) is an infectious disease containment unit developed by the Department of Defense that allows a limited number of infected patients to receive medical care in-flight while minimizing risk to aircrew, medical attendants and the aircraft. Developed during the Ebola outbreak in 2014, the TIS was designed with a specific focus on contact isolation. Because of the airborne nature of coronavirus, the TIS has been modified to ensure the safe movement of Covid-19 patients.
According to AMC, the TIS provides limited capacity and capability (between two and four patients), and the policy is to provide treatment in-place (without moving patients) when possible. A TIS Force Package consists of one C-17, two TIS modules loaded in the back, a front-end aircrew, and medical support in the back consisting of an Aeromedical Evacuation, Critical Care Transport Team, an infectious disease team (with a doctor and a technician), and TIS operators.
“AMC has made the TIS available and ready to transport Covid patients in response to official requests for support,” said Captain Nikki Ferrara, a USAF Air Mobility Command spokesperson. “AMC has pre-positioned two TIS Force Packages at Ramstein Air Base in Germany, in co-ordination with the US Transportation Command, to support potential Covid-19 requirements for movement of afflicted military forces in Europe, Africa and the Middle East.”
On 27 April, AMC began pre-positioning a TIS Force Package at Travis Air Force Base, California, consisting of two TIS units aboard a C-17 supported by aircrew and medical specialists. This West Coast-based TIS staging will eventually include 4 TIS Force Packages enabling AMC to more readily respond to requests to move patients in the Indo-Pacific Command region who may be afflicted with a contagion like Covid-19.
“When the coronavirus pandemic kicked off, the TIS was the only capability we had ‘in stock’ to transport Covid-positive patients, and that capacity was limited to moving a handful of patients at a time. While we ramped up training on that system and grew the number of TIS in our inventory, Air Mobility Command went looking for ways to provide greater capacity to move higher volumes of patients,” explained Ferrara. “With the understanding we’ll likely be dealing with Covid for some time, with frequent requests to move larger number of patients than what the TIS can handle, AMC collaborated with nearly a dozen other organizations from academia to private industry to DoD to develop the Negatively-Pressurized Conex (NPC), and in less than 30 days, it went from an idea on a napkin to a proven concept.”
The NPC is an isolated containment chamber fabricated from an actual steel Conex shipping container that uses fans continuously pulling the air from within the unit through high-efficiency particulate filters to prevent any exposure to the aircraft
The NPC is an isolated containment chamber fabricated from an actual steel Conex shipping container that uses fans continuously pulling the air from within the unit through high-efficiency particulate filters to prevent any exposure to the aircraft.
Ferrara added, “AMC is now moving forward with full production and rapid procurement of this new capability, with the potential to purchase up to 60 NPCs, including 30 full-size NPCs for inter-theatre transport on our C-17 and C-5 aircraft, and another 30 NPC-lite units, which are made-from-scratch aluminum Conex containers built on a pallet that fits comfortably inside a C-130 Hercules aircraft. The NPC-lite will be used for intra-theatre movement of Covid patients.”
The NPC can hold up to 28 passengers, 24 ambulatory patients, and / or up to eight litters. The NPC-lite will carry slightly less than that. The cost of the prototype and testing requirements was approximately US$2 million, and each NPC is anticipated to cost less than $800,000.

One of the newest and most immersive aeromedical trainers in existence is built by CAE. Their Aeromedical Evacuation Training System has been built to replicate C-130, C-17 and KC-135 fuselages configured for aeromedical evacuation missions. In use with the US Air Force Reserve Command, the system is designed to train flight nurses and aeromedical evacuation technicians for clinical proficiency and continuation training.
“The system allows us to train for in-flight clinical skills like medical assessment and treatment, and it also allows us to train for aircrew skills like rehearsal of aircraft emergencies like fuselage fire, smoke in the cabin, door warnings and rapid decompressions – anything that can cause a danger or threat to the patients or crew on the aircraft,” said Lieutenant-Colonel Chad Corliss, Deputy Commander of the 94th Aeromedical Evacuation Squadron, part of the 94th Airlift Wing.
“We could do clinical training with a patient sitting on a table, but simulating a patient at altitude at 30,000 feet, in the darkness, with the noise, and with the motion and turbulence from the AETD [Aeromedical Evacuation Training Device] motion generator allows our crews to suspend all disbelief such that we can treat high-fidelity human patient simulators in a representative environment as though they are real people,” explained Corliss. “The AETD allows us to take mission-ready qualified aircrew members and train them more effectively and more efficiently than ever before. The training opportunities are endless as we’ll have AETD systems for the C-17 and KC-135, which are other aircraft currently in use in the aeromedical system for the US Air Force.”
The AETD allows us to take mission-ready qualified aircrew members and train them more effectively and more efficiently than ever before
CAE’s Aeromedical Evacuation Training System can be developed for a range of air mobility aircraft platforms as noted above, as well as for rotary-wing aircraft. “We are pleased to partner with the US Air Force to provide the world’s first motion-based aeromedical trainer that will help ensure aeromedical aircrews are fully prepared for the critical aeromedical evacuation mission,” said Ray Duquette, President and General Manager, CAE USA. “The combination of our experience providing training solutions for air mobility platforms and CAE Healthcare’s world-class medical patient simulators demonstrates the unique training systems integration capabilities that CAE can deliver.”
New challenges, new solutions
With Covid-19 set to stay around for the foreseeable future, the need for ongoing improvement and development of patient isolation systems that can allow for critical care interventions continues, and the demand for these systems will also rise. However, there will always be new challenges on the horizon for aeromedical providers around the world, and the innovative solutions that medical equipment manufacturers and training providers can come up with will continue to fulfill the demands being made by operators and clinicians. Advancements made in the world of simulators, too, will continue to improve the realism that trainers need – putting the doctors and nurses under pressure to perform to the best of their ability, no matter what condition they are faced with.
ISOVAC CAPSULS – Adaptability is key to success - sponsored content
Classified and regulated as a Class ll Medical Device by the US Food and Drug Administration, the ISOVAC CAPSULS provides our customers the reassurance and reliability of regulatory oversight.
ISOVAC has collaborated with SPECTRUM Aeromed, the designers and developers of air ambulance medical interiors and equipment. ISOVAC CAPSULS, along with the Spectrum Aeromed equipment, can be accommodated in fixed- and rotary-wing aircraft in a multitude of sizes. The CAPSULS design facilitates the ease of the aircraft patient loading process prior to transport.
One of ISOVAC’s main goals is to save as many lives as possible. By designing CAPSULS with the flexibility and structure to accommodate treatment for a diverse range of patients of various ages, sizes, and statures, our system offers a versatile medical product that allows treatment during the MEDEVAC process.
COVID-19 has shown the world how ill-prepared they were to handle the containment and transport needs during the pandemic. With the recent surge of Covid-19 cases, compounded by the seasonal influenza, the continued need for the ISOVAC CAPSULS patient isolation unit is as important as ever. The Spanish flu, Asian Flu, Swine Flu, Ebola, and Covid-19 … if history has taught us anything, there will be future pandemics. Are you prepared?
November 2020
Issue
Innovations in critical care: The latest equipment and treatment options
Introducing IFR into HEMS operations: Planning and training are key
SAR equipment selection: Is there such a thing as the ‘right’ kit?
Electronic flight bags: Practicalities of use
Interview: Kolby Kolbet, LifeLink III VP Clinical Operations
Covid-19 in LATAM: Two providers share their experiences
Provider Profile: RACQ CQ Rescue
Dr Joetey Attariwala
Dr Attariwala trained as a medical doctor and has established himself as a highly regarded journalist who contributes to various aerospace, defense, training and simulation, and law enforcement publications around the world. He is a regular contributor to AirMed&Rescue magazine.


