Interview: Dr Julian Wijesuriya, KSSAA

AirMed&Rescue spoke to Dr Julian Wijesuriya, KSS Doctor and UCLH Consultant Anaesthetist, about the new interactive online training course for airway management
Airway Matters – the Trust’s Massive Open Online Course (MOOC) has attracted over 30,000 learners from 165 countries since launching in 2020. Could you tell us more about what the course involves?
Airway Matters is a free interactive online course that brings together frontline clinicians, leading international experts and patients to create a unique learning environment exploring the technical and non-technical strategies supporting safe airway management.
The course was launched in 2020 primarily as a hospital-based project, but in response to learner feedback, a team of experienced paramedics and doctors from Air Ambulance Charity Kent Surrey Sussex (KSS) developed a week of pre-hospital content.
Airway Matters is now a six-week course comprised of 15 to 20-minute bitesize steps that are grouped into themed weeks. Learning material is presented as articles, interactive images, presentations, videos and quizzes. There are also links to references and additional online resources and all the media content is downloadable for learners to refer to after the course.
The course is aimed at and attracts multi-disciplinary learners from a wide range of professional and specialty backgrounds, who engage with each other and the course via online discussion boards. The whole course is facilitated online by a faculty of experts from UCLH and KSS, who support learners through the weeks.
How does collaboration between emergency medical professionals enhance patient outcomes – can you share any concrete examples of where this happened?
Collaboration between emergency medical professionals is pivotal in enhancing patient outcomes. We have seen this clearly in the evolution of major transfer networks in the UK, where organizations and services have worked together within networks to organize and integrate care from the point of injury through to hospital discharge. National audit data has demonstrated that 20 per cent more patients are surviving severe injuries since the development of Trauma Networks; and KSS is proud to be part of and support three such networks.
On an individual patient basis, collaboration between emergency medical professionals is equally essential. KSS cares for critically ill patients, in complex environments, as part of a wider team of emergency services. We witness on a daily basis the benefit to patients of teamwork, effective communication and shared decision making.
From an education perspective, Airway Matters is a great example of what innovative organizations can achieve when they collaborate. The course allows experience and practice to be shared for the benefit of patients around the world.
How has the care provided by KSS medics changed lately – are you introducing new equipment or protocols for patient care?
Our most recent development is the introduction of Invasive Arterial Blood Pressure (IABP) monitoring. This provides continuous beat-to-beat information about a patient’s cardiovascular status. When looking after critically ill or injured patients, this information enhances our ability to provide advanced organ support and titrate our treatments even more accurately.
The equipment we use is Leadercath Arterial single lumen arterial catheter or Arterial SWiTCH FEP safety arterial cannula with wings, both manufactured by Vygon (UK) Ltd, and the Tempus Pro Monitor by Koninklijke Philips N.V.
In March 2020, KSS became the first HEMS to be rated Outstanding by the Care Quality Commission (CQC) in all five of its inspection key lines of enquiry: safe, effective, caring, responsive and well-led. How did you manage to achieve this?
We were proud to receive this Outstanding rating – a level only achieved by a very small proportion of the UK’s healthcare organisations. The report highlighted a wide range of exemplary practices at KSS including our ‘strong leadership’, ‘thoroughly patient focused team’, ‘open culture to reporting all types of incidents’, ‘highly motivated staff’ and ‘strong, comprehensive systems and processes’.
Our collaborative approach with local, national and international partner organizations to help improve services to patients was also singled out. The CQC also commended our commitment to our local communities, which is integral to how our services are planned and ensures that we meet the needs of the people we serve.
Overall, we have a culture of candor, reflection, governance and continuous learning and development, which underpins everything that we do and ensures that we are always striving to deliver the very best care to our patients.
How has flying 24 hours a day changed the ways in which KSS operates from a logistical point of view? Is it always the same standard crew set-up onboard no matter what time of day or night?
KSS was the first Helicopter Emergency Medical Service (HEMS) in the country to operate 24 hours a day, seven days a week. For 18 hours a day, we operate with two crews; for the remaining six, when it is quieter, we operate with one crew; and we always staff the crews with the same set up of an experienced doctor-paramedic team.
Establishing a 24-hour flying service required considerable challenges to be overcome, but has brought huge benefits to our patients – particularly the ability to rapidly convey critically ill patients over long distances to specialist hospitals at night.
Thanks to the generous donations of our supporters, we have been able to move to two AgustaWestland AW169 aircraft, which have a greater range and are more night capable. We also have specialist pilots, who train and maintain competence in night operations and ensure that our night aviation is safe. Our clinical teams have been trained in night HEMS operations, including the use of night vision goggles; and our dispatchers have protocols to dispatch the aircraft to presurveyed night landing sites, when appropriate, in order to expedite our arrival on scene.

What piece of medical kit would you say you value the most in your kit bag?
That’s a tricky one. We carry so much important and life-saving equipment and each component plays an irreplaceable role when needed. The patient monitor and stethoscope are two pieces of kit that we use on every single patient and help support our assessment and ongoing monitoring of them – so perhaps I would say those.
How has your career to date brought you to your current role?
I trained at Newcastle Medical School and as a junior doctor rapidly developed a passion for emergency medicine, critical care and anesthesia.
During my years of specialist training in anesthesia and intensive care medicine, I gained experience in a number of clinical and organization settings including aeromedical retrieval medicine in Queensland, Australia, and trauma medicine in an area of military conflict. I also undertook my first post at KSS as a HEMS registrar, which was pivotal for me. Thanks to the continuous training and support at KSS, I developed clinically and personally more than at any other time in my career, and the placement confirmed that I wanted to pursue pre-hospital emergency medicine long-term.
In my final stages of training, I maintained a commitment to pre-hospital care, advanced airway management and education, and I was honoured to be appointed as a Consultant Anaesthetist at the Royal National ENT Hospital, UCLH, and as a HEMS Doctor at KSS.
What do you find to be the most challenging part of your job with KSS, and what do you enjoy the most?
The most challenging part of my job is seeing people in pain or distress. We have to develop coping strategies on scene to ensure that we are always delivering the best care for our patients, but we depend on each other at KSS for support and to be able to debrief. It is a privilege to work at KSS, where I am always surrounded by such great colleagues. The most rewarding time for me is when a patient returns to visit us and we learn about their journey and the effect KSS’s care has had.
May 2022
Issue
In this issue:
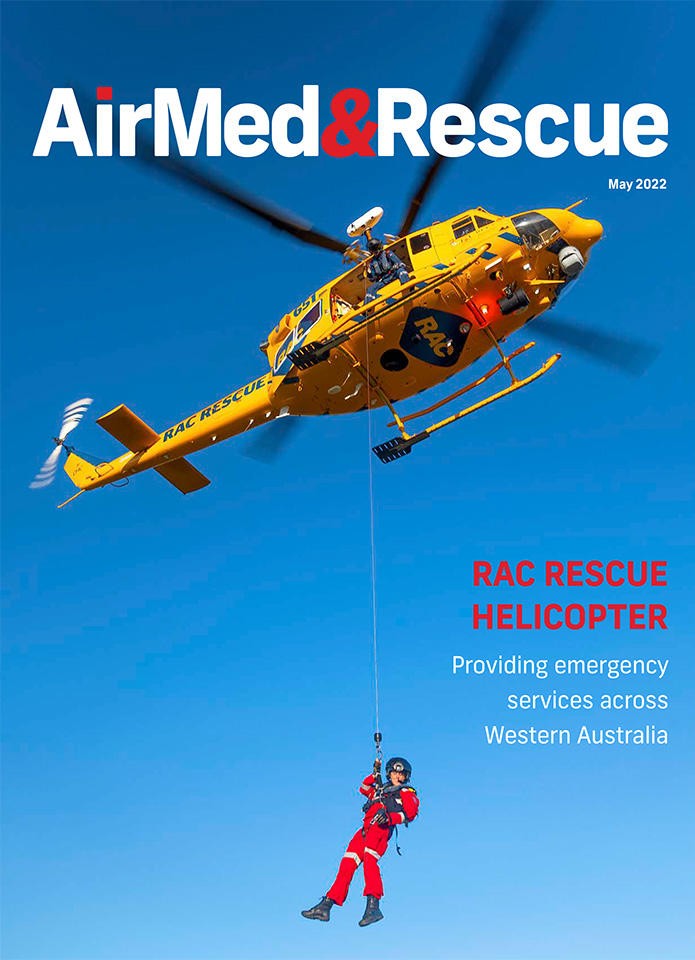
Dynamic hoisting; wireless communication solutions enhancing crew coordination; we say au revoir to the RCAF CC-115; introducing pre-hospital ECMO - nationwide coverage in the Netherlands; CAMTS' Executive Director Eileen Frazer looks at what critical care means; HEMS pilot Mike Biasatti explains how hard work and dedication pay off; and Dr Julian Wijesuriya on Airway Management interactive online learning course.
Editorial Team
The AirMed&Rescue Editorial Team works on the website to ensure timely and relevant news is online every day. With extensive experience and in-depth knowledge of the air medical and air rescue industries, the team is ready to respond to breaking industry news and investigate topics of interest to our readers.



