Interview: Dr Duncan Bootland, Medical Director, Air Ambulance Kent Surrey Sussex

Mandy Langfield spoke to Dr Duncan Bootland, Medical Director of Air Ambulance Kent Surrey Sussex in the UK, about how medical care onboard helicopters has changed for the better, and why ongoing research and education is key to keeping standards of care as high as they can be
How long have you worked for Air Ambulance Kent Surrey Sussex (KSS)? What are your key responsibilities in your new role of Medical Director?
I have worked for KSS since May 2012, first on a full-time secondment from my NHS Consultant post and then with a role split between the NHS and KSS.
As Medical Director, I have responsibility for the care we provide to our patients and have overall responsibility for the doctors within the service. It’s my role to ensure that we maintain the highest standards of care through our clinical governance process and that we are always striving to deliver the most up-to-date and effective care. At KSS, we are fortunate to have a group of highly skilled and passionate paramedics and doctors, and I see my role as harnessing the skills of the team to provide the very best for our patients.
KSS is an independent charity, and my role isn’t just limited to the clinical aspects of what we do. To be able to provide the care we do is a result of a huge operation in terms of income generation and community and stakeholder engagement, and I work alongside the other directors of the organisation as part of the senior leadership team. Working within that team, I help guide our strategy and long-term planning, and am the medical conduit to the Board of Trustees.
What are the biggest challenges KSS faces right now from a medical point of view, and how are you planning to overcome them?
Currently, Covid-19 is our biggest challenge; it has impacted almost every aspect of the medical care we provide. Through an enormous effort at the start of the pandemic, we looked at every part of our clinical operation and assessed how we needed to change. Perhaps the largest part of that has been the requirements for working in PPE. This has changed how we work, and particularly our ability to communicate on scene.
Our normal practice is to train through regular simulation both to ensure we’re at the top of our game in the way we care for patients, but also so we can ‘stress test’ new ways of working. We are fortunate to have a dedicated training area at our base, including an aircraft cabin simulator, and we have used this even more extensively over the last 10 months to test our processes and work out the best ways of working and communicating on scene.
Our normal practice is to train through regular simulation both to ensure we’re at the top of our game in the way we care for patients, but also so we can ‘stress test’ new ways of working
KSS was the first 24/7 HEMS in the UK. Why do you think most other charities haven’t yet made the move to 24/7 operations, despite the benefits to patients?
I don’t think the logistical challenges of operating a HEMS service at night, in terms of the aviation, the medicine and the additional fundraising that is required should be underestimated. I’m confident we’ve shown, over the last seven years, that there is a clinical need for us to operate 24/7 in our region. Each HEMS service will need to take a view on where the clinical benefit versus risk balance lies for their population, but I’m certain it was the right decision for us. We have significant transport distances to reach specialist major trauma centers, so night flying made sense for our patient population. We are extremely proud to be able to provide a 24/7 service.

Both of KSS’s AW169s together
When considering moving to 24/7 operations, were there any key lessons you learnt from other operators?
Given we have a significant number of ex-military pilots working for us, we were able to draw on their experience and knowledge, particularly in terms of what was achievable within the regulations with regard to weather and geography. Naturally, we liaised closely with the Civil Aviation Authority to ensure what we were doing was both safe and acceptable to them. We also undertook detailed prospective research to carefully evaluate the patient need overnight.
In terms of medical care onboard the helicopter, what do you see as the most important changes that have meant advancements in treatments and better outcomes for patients in the last five years?
I’d say our carrying of blood products, both red blood cells and plasma, over the last seven years has been the biggest change to the care that we provide, and this is something we do both on-scene and in flight. It is not as simple as choosing to carry the products; it comes with a significant learning curve in when, how and to whom to give the products.
In the future, do you think point-of-care diagnostic tools will become more prevalent in HEMS, and the ability to send this patient information to the hospital before the helicopter arrives at A&E will mean more efficient care can be offered by the NHS?
Absolutely. KSS has done a fantastic job of bringing high-quality emergency and critical care to the scene. However, one area we want to improve in terms of our on-scene care is diagnostics. Sharing the information we’re getting on-scene, such as blood pressure and oxygen saturation levels, is something that we can already do using the Philips Tempus Pro monitor with Corsium software. We were the first HEMS service in the world to use this, and this is something we’ve already seen the benefit of.
What does the AW169 mean in terms of enhanced patient care in the air?
The most obvious difference for us as a crew is the added cabin space and therefore the potential to do more whilst transferring the patient to hospital. Providing in-flight care, such as in-flight blood transfusion, has always been part of what we’ve done, but the added space makes that easier and provides other options for us to explore in the future. Add to that the additional aviation capabilities of the AW169, and certainly it’s a real asset to us.
What are your hopes for the future of air ambulance charity operations in the UK?
I hope ever more sharing of best practice between air ambulances will allow us all to learn from each other and so deliver even better care. Charitable funding affords us such operational agility, and I feel it’s a model that really serves the needs of the patients we attend. Equally, I love being a part of a service that is closely linked to the community we serve.
KSS, like other UK air ambulances, was founded through philanthropy, and we’re reliant upon the generosity of the community to deliver our life-saving service. Even though the current Covid crisis has meant unprecedented fundraising challenges, we’ve managed through incredible support from our community to continue supporting the NHS at a time when that’s never been more valuable.
I think most of us would agree the government support that we receive at the moment is gratefully received, but I hope that we will always remain a charity.
January 2020
Issue
In this issue
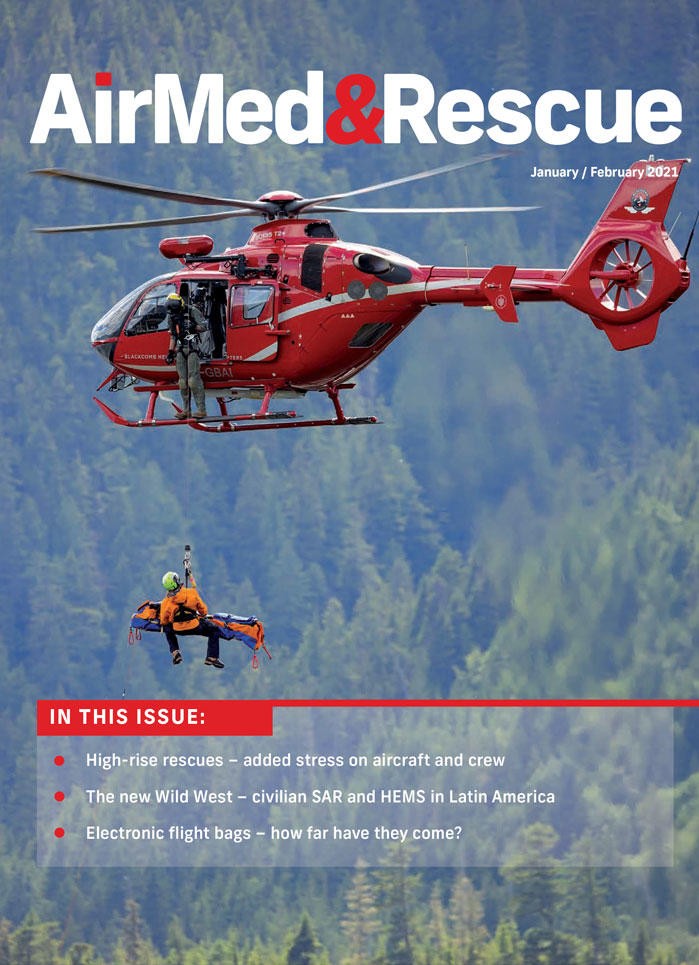
- High-rise rescues: added stress on aircraft and crew
- The new Wild West: civilian SAR and HEMS in Latin America
- Electronic flight bags: how far have they come?
- Interview with Dr Duncan Bootland, Medical Director, AA Kent, Surrey Sussex
- Research into point of care tools for diagnosis
- EURAMI accreditation during Covid-19
Mandy Langfield
Mandy Langfield is Director of Publishing for Voyageur Publishing & Events. She was Editor of AirMed&Rescue from December 2017 until April 2021. Her favourite helicopter is the Chinook, having grown up near an RAF training ground!

