Interview: Anna Van Der Werf, Flight Nurse, Royal Flying Doctor Service

Following an 18-year career with the Royal Flying Doctors Service (RDFS), Anna Van der Werf reflects on her experiences in her role as a Flight Nurse
Congratulations Anna! You have spent 18 years as a flight nurse, how did you end up working for the RFDS Western Australia?
We, my husband and I, migrated to Australia from the Netherlands after having completed my Registered Nurse/Midwife (RN/RM) training there. In Australia the opportunities are endless and varied as a RN/RM and I soon found myself working as a Remote Area Nurse (RAN), gaining first hand experience in Emergency Care, Anaesthetics and Midwifery.
This health care is vital for the people that live, work and travel in rural and remote Australia
I loved RAN in the Aboriginal Communities and Remote Rural Australia. That's when I first came across the Flying Doctors service. The RFDS was the first port of call for my patients’ consultations, and for the evacuations out of the remote area to a more suitable destination. I realised how limited the access to healthcare can be in rural and remote Australia, with all the specialist care located in the bigger cities, such as orthopaedics, cardiology, obstetrics, and mental health just to name a few. After a considerable time as a RAN, I decided it was time to look at the other side of the fence, and instead of having to call RFDS I was now the Flight Nurse (FN) on the RFDS plane to care for the patients in flight. That's how I ended up working for the RFDS and loving it.
Australia is a vast country which means isolated communities have limited access to healthcare and face long wait times in emergencies, how does this challenge motivate the RFDS?
RFDS is a 90-year-old non-profit organization that believes no matter where people live, they deserve access to skilled health professionals in their time of need. It is a privilege to look after the patients’ health during their emergency needs whilst flying them to specialist care. Dedicated teams of pilots, doctors, and Flight Nurses, spread out over different bases all over Australia respond to call outs dispatched from centralised call centres. Due to the vastness of the land the days can be long and varied. The challenge is always to meet the demands, to get to the sickest patients first in a timely manner and provide the appropriate health care needed for a good outcome. This health care is vital for the people that live, work and travel in rural and remote Australia.
What is unique about the role, in terms of both practically day to day, and what is required from a member of the team?
Nowhere else in Health Care do you have a view from your office window as you do from a RFDS plane. The uniqueness is the very small team you work with, and the isolated places you go to. It can be just the pilot and yourself as the Flight Nurse, and at times there will also be the one Doctor on the flight. In the PC12 we can have two stretcher patients and one sitting one. There are the extreme temperatures to deal with, the area to work in is very confined, it can be noisy, all the equipment needs to be secured. There are altitude pressures to deal with, and turbulence in flight. The turbulence can be scary and uncomfortable for the patients and a lot of reassurance is needed.

What has been the most challenging call you have attended and why?
The most challenging call out was to multiple wounded patients and only having limited resources of staff and equipment. Only the Doctor, pilot and I were called out to a small plane crash in a very remote area. There were six occupants on the plane, and on arrival on the small dirt airstrip we had to make a lot of immediate decisions such as what equipment to take off the plane to go in the back of a Ute, that was going to take us through the bush to the crash site. The safety of all had to be thought of as there was leaking fuel around the crash site, the wounded were spread out, and two patients unfortunately did not survive, including a nine-month-old baby. Our thoughts though had to go to the wounded and who to care for first, and then transport them with the Ute back to the RFDS plane, one at the time. We were also time limited, to get out of there before dark, as the airstrip had no lights. The pilot definitely had to multitask as part of our small health care team.
What has been the most memorable call out for all the right reasons?
The pilot and myself had gone out on an uncomplicated patient pick up when we were diverted in flight. We had to go to a small isolated rural town that was without a doctor or midwife. There was a woman in labor at 36 weeks gestation that needed to be transferred. On arrival I was taken to the small health care building where I found the patient to be in full labor and about to give birth. It was a wonderful outcome and to be able to assist the women in delivering her healthy baby girl was a very happy occasion. We then transferred mother and baby onto the plane to the appropriate town for obstetric and pediatric check-ups and a short stay.
The thing I will miss the most is being part of that unique team that helps the wonderful people of remote Australia to get the best outcomes

In terms of aircraft, what has been your experience over the years of both capabilities and medical advancements on board?
The capabilities of the aircraft from a pilot’s point of view have definitely improved over the years. The new technology in our latest aircraft is very important for our pilots as they have to be very skilled to land the planes on remote dirt airstrips, which can be very challenging especially at night time. Beside our fleet of Pilatus PC12's and in other states in Australia, King airs, RFDS do now have Jets (PC24) as well which is making a huge different for our patients. We can get to our patients much quicker in an emergency and also carry more patients (three stretchers). On board advancement include improved stretchers for comfort, specialised PC12 obese stretchers again for comfort and excess, and improved neonatal cots.
Flight nurses are highly skilled at dealing with in-flight medical emergencies, what is a flight nurse’s role during the unlikely event of an aircraft emergency?
We have regular drills for aircraft emergencies, we do cabin safety training, dangerous goods courses, and emergency landings drills. We have training on how to get out of the plane via emergency exits, know where all the emergency equipment is on the plane, how to assist the pilot and know how to work the radio.
What will you miss the most about working for the RDFS Western Australia?
The thing I will miss the most is being part of that unique team that helps the wonderful people of remote Australia to achieve the best outcomes. Patients are always so grateful when the RFDS arrives, knowing they can get the skilled and safe in flight care they need in order to access specialist care. I will miss flying over the great Australian Outback, and the sight of the beautiful night skies.
October 2022
Issue
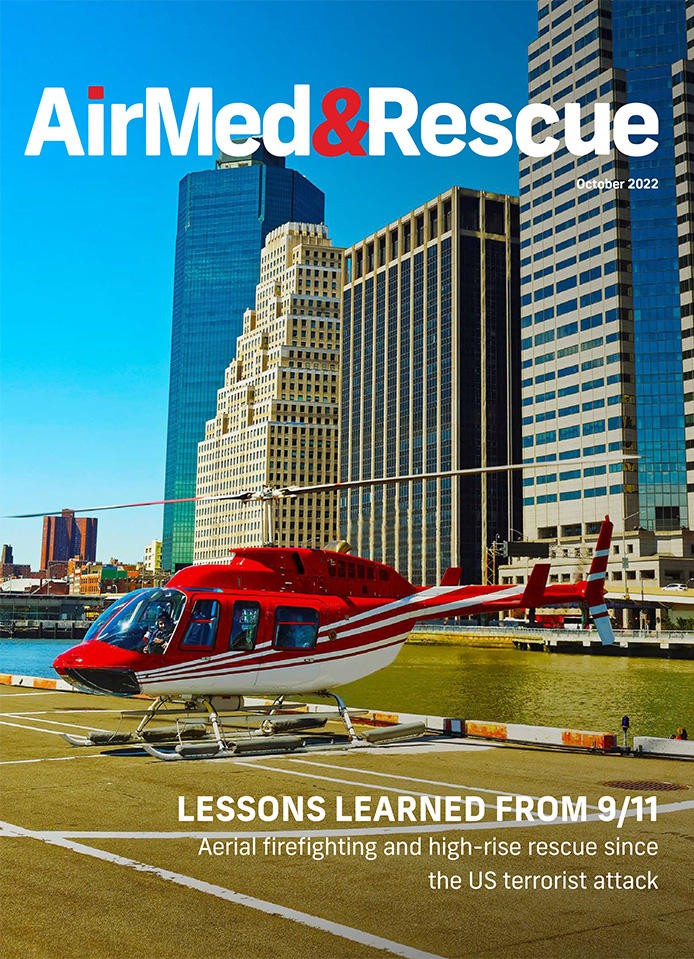
Aerial firefighting and SAR after 9/11; innovative use of stroke scanners by the RFDS; European nations’ response to this summer’s intense wildfire season; and the ongoing evolution of night vision systems, all in the latest issue. Plus, the USHST and EASA share regulatory updates on safety measures for operators, and the European Rescue Swimmers’ Association tells us what’s coming up at their next event
Editorial Team
The AirMed&Rescue Editorial Team works on the website to ensure timely and relevant news is online every day. With extensive experience and in-depth knowledge of the air medical and air rescue industries, the team is ready to respond to breaking industry news and investigate topics of interest to our readers.



