End of life repatriation flights - ethical challenges for air ambulance providers

Typically, in civilian fixed-wing air ambulance flights, patients are being taken home so that they can be helped to live. Some missions, however, confront operators with ethical rather than medical challenges: taking patients – often comatose – home to die. David Kernek explores some of the issues surrounding these missions
So-called ‘end-of-life’ repatriation flights are the most complicated type of case an air ambulance provider can handle, explained Dr Hervé Raffin, managing director of Medic’Air International. In some cases, the company has to provide a quote, at short notice, when the exact date of the trip, and often therefore the status of the patient, may not be known. Also, the escorting medical team has to care for the patient during flight, providing comfort – but not resuscitation – to ensure the patient is alive when they reach their destination. He suggests that such patients should be flown on private air ambulances, rather than as a stretcher on a commercial airline, due to the chance of death occurring in the air. For the same reason, Medic’Air International always requests that a family member is on the plane, as they can see how the medical team is working, and can better understand that the best was done for the patient.
Unusual ethics
The first issue to be resolved when considering an end of life repatriation flight may be an ethical one. Dr Joseph Lelo, chief medical officer for AMREF Flying Doctors, commented: “We are bound to act ethically as medical providers and we always put the interests of the patient first. We do strive to get the patient to a better level of care if possible. If we feel that the patient would not benefit or would not survive the transfer, we seek second opinions from senior doctors on the ground or from the intended destination to come up with a way forward.” He added: “We do find, in most cases, that the decision to transfer these patients has already been made by the patient themselves, relatives or by the medical insurer. Our part is to look at the logistics and determine if the transport is possible without causing further detriment to the patient.”
For Dr Jon Warwick, medical director of UK-based Air Medical Ltd (AirMed), the standard medical ethics and medical analyses may not apply to these missions: “Clinicians must always work according to the patient’s best interest, but if the patient is brain-dead and being managed on an intensive care unit abroad, there is no ‘patient’s best interest’ here; after all, they are already dead.” However, looking at the wider picture, the patient’s best interests – and those of their family – are not generally met by leaving them to die overseas, he said, even if they do not meet the standard ‘fit to fly’ criteria. He added: “What we are really dealing with is providing a good death for the people left behind, so they haven’t got the terrible angst for the rest of their lives because Uncle Joe was left to die in Istanbul.”
Whether or not AirMed accepts an end-of-life mission comes down to what Dr Warwick and his team deem not only medically, but also ethically, correct, he said: “[UK medical staff are] bound by terms of conduct as described by the General Medical Council in its guide Good Medical Practice. There is sometimes a careful balance to be made concerning the ethics of a transfer of the sick and dying. An air ambulance company must have a ‘moral compass’ of what it considers to be acceptable, even though it is appreciated that others might hold a contrary view. Any patient or family will always find someone who is willing to fly them anywhere, since there might be money to be made; as an air ambulance company, the question is, should we?”
if the patient is brain-dead and being managed on an intensive care unit abroad, there is no 'patient's best interest'
Dr François-Xavier Duchateau, initiative medical manager at Allianz Global Assistance, agreed that a patient might not by normal standards be fit to fly, but explained: “In some circumstances, this can be outweighed by their wish to die in their home country. There is a risk that the patient might die during the air ambulance flight, but there is a strong compulsion in some patients to die in their home country. And for families of people who might die while they’re abroad, it must be very difficult and additionally stressful, which is why I say the main reason for such flights is one of compassion … it’s for psychological and emotional reasons.”
Hoping for a miracle
One of the challenges air ambulance operators must deal with is the family of a terminally ill patient that harbours hopes of a recovery after repatriation to their home country, when in reality all that is possible would be a well-managed death.
Tiina Kauhanen, AirMed’s deputy chief flight nurse, reflected: “We would have a really frank discussion in advance with the insurance company to make sure what the family knows. If we’re not happy with the information we get from the insurance company, we ask for the next-of-kin’s phone number, and we call them and ask what they know and what they expect. We want to make sure that their expectations are in line with what we’re going to provide, which might not be a return to the UK for a miracle cure … We will tell them frankly that if their relative dies during the flight, we will only keep him comfortable, we will not do any further medical treatment, and we want to be sure they understand this.”
Assistance companies and air ambulance teams have to make families aware of what’s possible and what isn’t when taking terminally ill patients back to countries in which life support is likely to be withdrawn, says Dr Duchateau. “No information of that kind should be hidden. Everything should be very transparent and clear. But we had a case in which the family was well aware of what would happen. The patient, for whom there was obviously no hope, was in Israel. The doctors there did not want to stop support, but the family asked us to bring the patient back to France, where they knew support would be withdrawn.”
When to say no
There are limits to accepting end-of-life repatriation missions, according to Dr Duchateau: “There is no such thing as two identical cases, so there are case-by-case discussions about the ethical and logistical concerns. This kind of patient, one with a very short-term prognosis, is sometimes very difficult to assess, even if they are conscious. The situation during the flight can be very changeable. Sometimes we have to be prepared to say ‘no, we can’t do it’. If I think there is the possibility of the patient dying in the next hour, I say the transportation cannot be done.”
East West Rescue of India organises air ambulance services from locations such as the Middle East and the Maldives to China and Southeast Asia. A representative commented: “When we receive a request for an end-of-life repatriation, the insurance or assistance company abroad is already aware of the patient’s condition and it has been in touch with the patient’s family or companion and made them aware of the risks of a transfer and the pros and cons of the patient’s current location. When our team arrives at site to carry out a repatriation, it evaluates the patient, informs the assistance/insurance company or a companion at site and has them sign a high-risk waiver.” East West Rescue said it might decline an end-of-life mission request if it involves both travel over international waters and a high risk of death during the flight, since this could lead to cumbersome paperwork.
Dr Warwick of AirMed described two cases that were put to his ethical test. Although superficially similar, one patient was flown while the other was declined: “Last year, we were asked to transfer a lady with advanced ovarian cancer from the south of Spain, where she lived as an expatriate, back to the UK in order to pass away at home. She was approaching the end of her life, and required some compassionate nursing care and an air ambulance in order to make this possible. We undertook this transfer. The very next week, we encountered a very similar patient, in a UK hospital and suffering from a similar disease process; she was also at the very end of her life. She requested (via her family) an air ambulance to take her to a European clinic to undergo experimental stem cell treatment. Significantly, this was not with the agreement of her treating clinicians in the UK. We declined this transfer. The important difference is that this patient had very different expectations: she hoped, unrealistically, to survive and wanted the transfer to achieve that; the first patient had expectations to die. Another operator took the patient to the experimental clinic.”
Patrick Schomaker of European Air Ambulance (EAA), however, told Waypoint that generally, in cases where a patient wants to be flown in order to reach treatment, it is not the air ambulance company’s role to assess the suitability of that treatment. Such a patient would be dealt with as any other case – if they met the fitness to fly criteria and could be transported without risk, then they would be accepted.
Waivers and disclaimers
It’s these sorts of missions, suggested Dr Duchateau, that in some circumstances strip liability waivers and the fitness-to-fly criteria of meaning. “I’m not that crazy about forms about responsibilities and liability in these cases,” he said. “The main thing is to have a discussion with the patient or their family members, so that everyone is aware of the risks. Clearly, in many cases, the patient is not fit to fly, yet with these cases we are in a very different logic and perspective, so the fitness-to-fly concept is not really relevant.”
There is a discussion, he said, with the patients, or most often their relatives, about the risks involved in a transportation when the patient is not in the stable state normally needed for repatriation flights. “Then we say, OK, we’ll do the transportation, but the family have to be made very aware of the risks. Maybe a liability form can give the evidence that the patient or the family received the information and agreed to the flight. In my company and in France, a liability waiver is not something that’s important. The notion of fitness-to-fly is almost an irrelevance in the circumstances of many of these missions.”
Dr Warwick also considers liability and consent forms to be of limited, if any, legal use: “Only the patient (or their legal power of attorney, or parents in respect of their children) can give consent. Other well-meaning relatives cannot give consent on behalf of another adult, whether the adult has mental capacity or not. Getting relatives to sign ‘disclaimers’ is therefore largely irrelevant. It is the nature of the discussion, and most importantly its understanding, that is vital and must be clearly documented in advance by the air ambulance staff. Any transfer – indeed, any form of medical intervention – should always aim to gain the consensus agreement of family and clinicians.”
what we are really dealing with is providing a good death for the people left behind
AMREF Flying Doctors does have a consent/waiver form, said Dr Lelo, but he stressed that what is important is to disclose as much to the relatives as possible and to obtain informed consent. Patrick Schomaker of EAA said that while the company does have a document for the patient to sign (or for family members to sign, in the case of a patient who is incapacitated), EAA recognises that this is unlikely to provide a bullet-proof legal defence in the event of litigation. As Schomaker explained, a patient could later claim that they were pressured into signing, or were desperate enough to sign anything. However, echoing Duchateau’s comments, the document is an important tool used to make sure the patient and family are aware of the risks involved in a transport.
For Dr Raffin of Medic’Air International, the answer is clear: “We don’t ask patients or family members to sign any waivers, as they would have no value in French laws. Rather, we have to explain all the risk of complications during the evac to the familly, and must be able to prove that they fully understood our explanations and that they were in accordance with the transport risk.”
Light in the dark
So, end of life missions can be a benefit to the patient and/or their family by allowing them to die at home. Nonetheless, they can also be lifesaving, even in the case of brain-dead patients, as Dr Warwick noted: “It is possible, once returned [home] and brain death is confirmed, that the patient may be an organ donor candidate. Out of this tragedy, other lives might be saved.”
March 2016
Issue
In this issue:
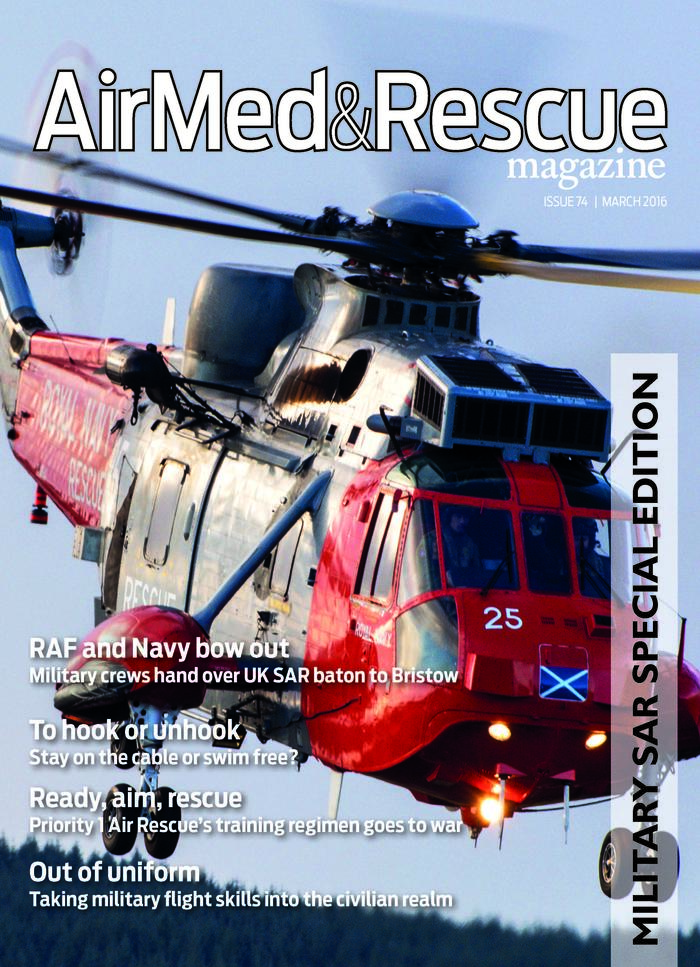
RAF and Navy bow out - Military crews hand over UK SAR baton to Bristow
To hook or unhook? Stay on the cable or swim free?
Ready, aim, rescue - Priority1AirRescue's training regimen goes to war
Crew resource management
Interview: Kevin Weller, Chief technical rearcrew, Bristow Helicopters, HM Coastguard Caenarfon SAR
Aircraft Spotlight: Quest Kodiak 100
David Kernek
David Kernek is a freelance writer and photographer who in recent years has been editor of Holiday Villas, Holiday Cottages and Go Holiday travel magazines. In an earlier life, he was the Westminster-based political correspondent of The Northern Echo and, later,editor of the Bath Chronicle, the York Evening Press and The Northern Echo. Moderately well-travelled, countries and regions he’s visited either for work or vacations include – from west to east – the US, Canada, St. Lucia, Ireland, most of western Europe, almost all of Greece, Turkey, Israel and South Korea. He hopes to see more of England.

