Case study: Rare case of agenesis of the corpus callosum in a neonate
Dr Ioannis Mamidakis, Medical Director for Gamma Air Medical, shares a case of a transportation of a neonatal patient with agenesis of the corpus callosum
The corpus callosum is the major pathway of fibers that connect the two encephalic hemispheres. Agenesis of the corpus callosum (ACC) is a rare disorder that is present at birth (congenital). The prevalence of the anomaly is approximately 1.4 per 10,000 live births and it has male predominance. There may be a partial or complete absence (agenesis) of this anatomic structure (which normally consists of 200 million neurons), the pathogenesis of which is not completely clear. It can be inherited as either an autosomal recessive character (chromosome 9 seems likely to be the one that causes the problem) or an X-linked dominant character. It is also possible to be caused by an infection during the 12th to the 22nd week of the intrauterine phase of life (during pregnancy) leading to this developmental disorder in the embryo’s brain. Intrauterine exposure to alcohol (fetal alcohol syndrome) can also result in ACC.
Case presentation
The patient was born in Albania in March 2023 at full term with a natural birth. SARS-CoV-2 infection was reported during the third month of gestation; both parents were healthy, and non-consanguineous. The child’s birth weight was 2.4kg; the Appearance, Pulse, Grimace, Activity and Respiration (APGAR) Score was 7–9 (hypotonic and cyanotic, crying after tactile stimulation); the patient presented with hypoglycemia with tremor and unspecified convulsions; and had neonatal jaundice that was treated with phototherapy. The neonate also had difficulty swallowing and sucking, and presented with desaturation; oxygen support was necessary. The patient remained hospitalized in the neonatal intensive care unit (NICU) in Tirana for one month due to an unspecified infection. A computed tomography of the brain was performed that showed ACC without other obvious lesions. Laryngomalacia and bilateral paralysis of the vocal cords were also diagnosed.
The baby was transferred to a specialized center in Rome, Italy, for further evaluation and continuation of treatment. In July, a magnetic resonance imaging of the brain was performed that showed a reduction in volume of the brainstem with an increase in the width of the basal cisterns, marked reduction in thickness of the white matter in the bilateral temporo-parieto-occipital area, and confirmed the presence of ACC. In August 2023, given the swallowing difficulties and the poor growth, a percutaneous endoscopic gastrostomy (PEG) was put in place. In September, the patient was transferred to the ICU of a hospital in Rome due to persistence of stridor and severe desaturation even while receiving oxygen therapy. After various attempts of non-invasive ventilation, the patient underwent rhinotracheal intubation (size 3.5 without cuff) and mechanical ventilation started.
In October 2023, Gamma Air Medical, based in Athens, Greece, received a request for the air medical transportation of the patient from Rome to Tirana, Albania.

Preparation and execution of the flight
Once the operations department of our company received the request for the repatriation of the patient back to Tirana, we tried to collect as much information as possible regarding the medical status of the child. We contacted the Roman hospital and spoke with the treating doctors of the ICU. We received important details concerning the situation: medications protocol with doses, ventilator settings, number and type of tubes and drainages, and relative’s escort details with copies of the travel documents made available to the medical director.
This information was very important in order to decide on the medical team; for the medical equipment to be set up, the flight details to be arranged, and the ground transportation to be booked in accordance to the flight plan; and all necessary permissions from local aviation authorities to be granted. According to the plan that had been devised and given the serious condition of the patient, our medical team consisted of two physicians (Dr A Ntouzepi, a pediatric anesthesiologist, and Dr I Mamidakis, the medical director) rather than our standard crew of a registered nurse and physician.
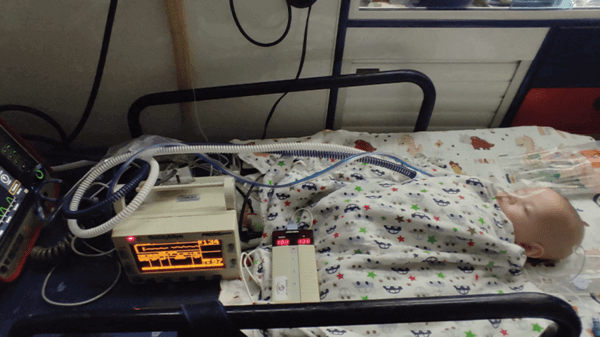
We supposed that both of us would pick up the child from the hospital in Rome and would accompany the patient up to the hospital in Tirana; however, the patient arrived at Rome airport direct with an ambulance and an accompanying anesthesiologist. The patient was then transferred from the ambulance’s stretcher to the aircraft’s stretcher with care and diligence, avoiding any risk of disturbing the rhinotracheal tube from the patient’s airway. The patient (height of 60cm and weight of 4.5kg at the time of pick up) was mechanically ventilated under continuous mandatory ventilation (CMV) mode on a Hamilton T1 Ventilator in neonatal configuration, with positive end-expiratory pressure (PEEP) of 8mmH2O, tidal volume of 40mL, respiratory rate of 36 breaths/min, fraction of inspired oxygen (FiO2) of 45%, and sedated with fentanyl (5.7μg/kg/h) and midazolam (0.5mg/kg/h), hydrated with Normosol (2mL/h), fed through PEG with Infatrini Peptisorb (18mL/h), and kidney function supported with furosemide (2mg three times per day; the patient received the morning dose just before leaving the referring hospital). All intravenous medications were administered through our Injectomat MC Agilia Fresenius Kabi infusion pumps.

The flight, on a Beechcraft King Air 200, from Rome to Tirana was uneventful. The ventilator settings were kept substantially unchanged, the medication regimen was maintained unmodified, and the vital signs of the patient were under continuous monitoring (blood pressure of 85/45mmHg, heart rate with minimal fluctuations of 120–130bpm, oxygen saturation of 97–98%, and body temperature of 36.2°C).
The only slight modifications we decided to adopt once we reached the cruising altitude were the PEEP (from 8mmH2O to 5mmH2O), the respiratory rate (from 36 breaths/min to 30 breaths/min) and the hydration by adding 40mL of Ringer’s solution intravenously for the duration of the flight only (almost two hours). The urinary output for the duration of the flight was approximately 120mL.
Once we landed at Tirana airport, the ambulance we had arranged to take the patient and the local medical crew to the admitting hospital was waiting for us on the tarmac. The ambulance staff (an anesthesiologist and an intensive care nurse) received all the information from us regarding the patient. We checked the vehicle’s equipment and the sufficiency of the medical oxygen of the ambulance. At that point, we noticed that the ventilator that was equipped in the ground ambulance was not appropriate for such a small patient. Consequently, when we carefully disembarked the child and placed him into the vehicle’s stretcher, we did not disconnect the child from our portable ventilator. We maintained the patient connected to our device, and we kept the infusion pumps we carried with us in the flight on the child and departed with the ground ambulance. We soon arrived at Tirana hospital, where we transferred the patient to the medical staff of the ICU of the hospital without any other unforeseen events.
Conclusion
We follow a ‘golden rule’ that our experience and our dedication to this amazing and risky field has taught us: If we have to accompany a patient somewhere, we make preparations for two. Medical devices, batteries, oxygen and consumables, even clothing, are never enough; we must carry a backup in the event that there is a failure or something unforeseen occurs. Especially when we deal with the rarest cases in the air.

March 2024
Issue
In the March edition, get transported in flying medical units; see how digital cockpits can improve your workload; discover how different firefighters use different tools, equipment and craft; and discover the innovations and improvements to aerial firefighting coming out of the American west coast; plus more of our regular content.
Ioannis Mamidakis
Medical Director for Gamma Air Medical.

